When you're taking an ACE inhibitor like lisinopril or enalapril to control your blood pressure, you might not think twice about eating a banana or a baked potato. But for some people, those foods can quietly push potassium levels into dangerous territory - and that’s something your doctor might not have told you.
How ACE Inhibitors Affect Potassium
ACE inhibitors work by blocking a hormone called angiotensin II, which normally tightens blood vessels and raises blood pressure. But there’s a side effect you can’t ignore: they also reduce the production of aldosterone, a hormone that tells your kidneys to flush out excess potassium. When aldosterone drops, potassium builds up in your blood instead of being removed.This isn’t a glitch - it’s how the drug works. And while most people handle this fine, others can see their potassium levels climb fast. The average increase? Around 0.5 to 1.0 mmol/L for someone with healthy kidneys. But if you have kidney disease, diabetes, or are over 65, that jump can hit 1.5 to 2.5 mmol/L. That’s not just a number - it’s a ticking clock.
When potassium goes above 5.0 mmol/L, you’re in the danger zone. Above 6.0? That’s a medical emergency. Symptoms aren’t always obvious: muscle weakness, nausea, a fluttering heart, or even sudden chest pain. Some people feel nothing until their heart rhythm goes haywire. And in rare cases, it leads to cardiac arrest.
Which Foods Are the Biggest Risks?
You don’t need to avoid all potassium. But some foods pack a punch - and when you’re on an ACE inhibitor, they can tip the scale.- Bananas: One medium banana = 326 mg of potassium. Two a day? That’s 650 mg - more than many people get from their entire diet before.
- Avocados: Half an avocado = 507 mg. Popular in smoothies and salads, but a hidden risk.
- White and sweet potatoes: One medium baked potato = 670 mg. Topped with butter? Even worse if you’re using salt substitutes.
- Tomatoes and tomato products: Tomato sauce, paste, or juice can easily push 400-600 mg per serving.
- Dried fruits: Apricots, raisins, prunes - concentrated sugar and potassium. A small handful can add 300+ mg.
- Coconut water: One bottle = 1,500 mg. It’s marketed as a “healthy” drink, but it’s a known trigger for hospitalizations in people on ACE inhibitors.
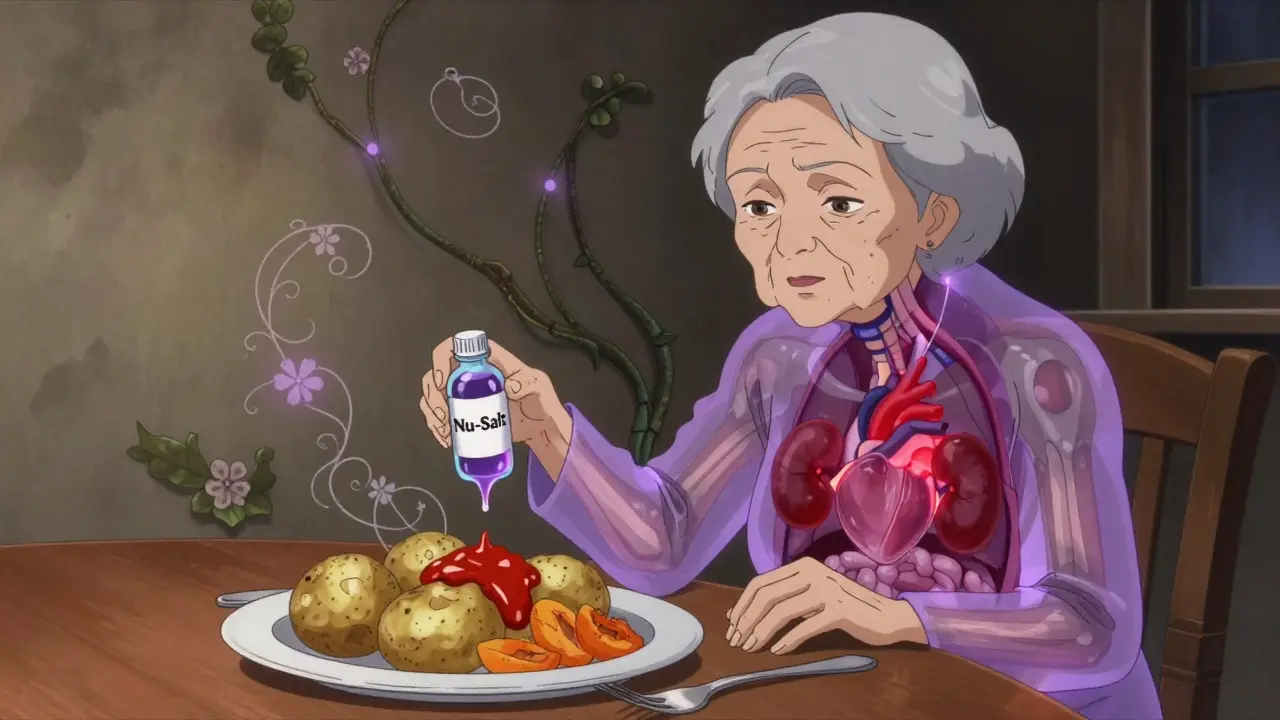
- Salt substitutes: Products like Nu-Salt or NoSalt replace sodium chloride with potassium chloride. One 1.25g scoop = 525 mg. If you’re trying to cut salt, this can backfire badly.
It’s not just about eating one high-potassium food. It’s about stacking them. A smoothie with banana, avocado, and coconut water? A meal with potatoes, tomato sauce, and a side of dried fruit? That’s how levels spike - slowly, silently.
Who’s at Highest Risk?
Not everyone on ACE inhibitors needs to change their diet. But if you fit any of these categories, you’re in the high-risk group:- Chronic kidney disease (CKD) stages 3 or 4: Your kidneys can’t flush potassium well. Risk jumps to nearly 13% per year.
- Diabetes: Even mild kidney damage from diabetes raises your risk 3.2 times.
- Age 65+: Kidney function naturally declines. Older adults often don’t notice early symptoms.
- Taking other potassium-raising drugs: Spironolactone, eplerenone, or trimethoprim? Combine those with ACE inhibitors, and your risk triples or quadruples.
- Low sodium intake: If you’re on a very low-salt diet, your body holds onto potassium more tightly.
And here’s the catch: many people don’t know they have early kidney damage. A routine blood test can catch it - but if you haven’t had one in over a year, you might be flying blind.
What the Experts Really Say
There’s disagreement among doctors - and it’s confusing.Some say: “Don’t worry. Studies show people with normal kidneys can safely eat 3,400-4,700 mg of potassium daily, even on ACE inhibitors.” That’s based on a 2016 JACC study. And yes, potassium has heart benefits - it helps lower blood pressure naturally.
But others warn: “In real-world practice, we see patients hospitalized after eating a few extra bananas or drinking coconut water daily.” One nurse on Reddit said she’s seen a dozen cases - all elderly, all with undiagnosed mild kidney disease.
The truth? It’s personal. Your doctor should be looking at your bloodwork, not giving blanket advice. If your last potassium test was normal, you’re likely fine with moderate intake. But if you’re over 65, have diabetes, or haven’t had a lab test in a year - you’re playing with fire.
What You Should Actually Do
Forget extreme restrictions. Focus on smart, practical steps:- Get tested: Ask for a basic metabolic panel (BMP) before starting an ACE inhibitor, then again at 1-2 weeks after starting or changing your dose. After that, every 3-6 months if you’re stable - monthly if you have kidney disease or diabetes.
- Know your numbers: Normal potassium is 3.5-5.0 mmol/L. Anything above 5.0 needs attention. Above 5.5? Call your doctor immediately.
- Space out your meals: Eating high-potassium foods 2 hours before or after your ACE inhibitor dose can reduce the spike by 25%. Timing matters.
- Watch the salt substitutes: If you’re using them, stop. Use herbs, lemon juice, or vinegar instead.
- Limit high-potassium foods to one serving per day: One banana, one potato, one avocado - not all of them. Avoid coconut water entirely if you’re at risk.
- Don’t take potassium supplements: Unless your doctor specifically prescribed them - which is rare if you’re on an ACE inhibitor.
There’s no need to give up avocados forever. But if you’re eating three servings a week, cut back to one. Swap sweet potatoes for regular white rice. Choose apple juice over orange juice. Small changes add up.

What About ARBs? Are They Safer?
Angiotensin II receptor blockers (ARBs) like losartan or valsartan work similarly to ACE inhibitors - but they’re slightly less likely to raise potassium. Studies show ARBs carry about 60% of the hyperkalemia risk of ACE inhibitors. So if you’ve had a potassium spike before, your doctor might switch you. But don’t assume ARBs are risk-free. They still affect aldosterone. The same dietary caution applies.What’s New in 2026?
New tools are making this easier to manage:- Genetic testing: A variation in the WNK1 gene can identify people who are genetically prone to hyperkalemia on ACE inhibitors. If you’ve had repeated high potassium levels, ask if genetic screening is available.
- Potassium binders: Drugs like patiromer (Veltassa) can bind potassium in your gut and remove it in your stool. Approved since 2015, they’re now used more often to let patients stay on ACE inhibitors without strict diet changes. In trials, 89% of people who couldn’t tolerate potassium-rich foods were able to resume them after starting patiromer.
- Remote monitoring: Some clinics now offer home potassium test kits. You prick your finger, send a sample by mail, and get results in 48 hours. A 2023 study showed this cut hospitalizations by 28%.
These aren’t magic fixes - but they mean you don’t have to choose between your meds and your favorite foods.
Bottom Line
You don’t need to live on plain rice and boiled chicken. But if you’re on an ACE inhibitor, ignoring potassium is dangerous. The key is awareness - not fear.Get your blood tested regularly. Know your numbers. Avoid stacking high-potassium foods. Skip salt substitutes. Talk to your doctor - not just about your blood pressure, but about your diet, your kidneys, and your risk.
Because the goal isn’t to avoid all potassium. It’s to keep your potassium safe - so your heart stays strong.
Can I still eat bananas if I’m on lisinopril?
Yes - but only if your potassium levels are normal and your kidneys are healthy. One banana a day is usually fine. Two or more, especially with other high-potassium foods, can be risky. If you have diabetes, kidney disease, or are over 65, limit it to once a week or less. Always check your last lab result before assuming it’s safe.
How often should I get my potassium checked on ACE inhibitors?
Before starting the medication, get a baseline test. Then check again at 1-2 weeks after starting or changing your dose. If your levels are stable and you have normal kidney function, check every 3-6 months. If you have diabetes, chronic kidney disease, or are over 65, check monthly. Many people skip these tests - but that’s when problems go unnoticed until it’s too late.
Do all ACE inhibitors raise potassium the same way?
No. Enalapril has been shown to carry a 15% higher risk of hyperkalemia than lisinopril at the same dose, likely because it stays in your system longer and penetrates tissues differently. Captopril and ramipril fall in between. If you’ve had a potassium spike before, ask your doctor if switching to lisinopril might lower your risk.
Is coconut water really that dangerous?
Yes - especially for older adults or those with kidney issues. One bottle of coconut water can contain 1,500 mg of potassium - more than four bananas. It’s marketed as a “healthy” drink, but it’s a common cause of hospitalizations in people on ACE inhibitors. Avoid it entirely if you’re at risk. Water or unsweetened tea are safer choices.
Can I use salt substitutes if I’m on an ACE inhibitor?
No. Most salt substitutes replace sodium chloride with potassium chloride. One small scoop (1.25g) contains 525 mg of potassium - nearly a third of your daily limit if you’re at risk. Even if you’re trying to cut salt, this can push your potassium into the danger zone. Use herbs, lemon, garlic, or vinegar instead.
What if my potassium is high - do I have to stop my ACE inhibitor?
Not necessarily. Many patients can stay on ACE inhibitors with the help of potassium-binding medications like patiromer (Veltassa), which removes excess potassium from your gut. Your doctor might also adjust your dose, switch you to an ARB, or treat the underlying cause (like kidney disease). Never stop your medication on your own - but do get it checked immediately if your potassium is above 5.5.

