AGEP Trigger Timeline Tool
Choose a medication and click "Show Timeline" to see the expected onset period for AGEP.
Imagine waking up with your skin covered in tiny white bumps, burning and itching, just two days after taking a common antibiotic. You might think it’s a mild allergy - but it’s not. This could be Acute Generalized Exanthematous Pustulosis (AGEP), a rare but dangerous skin reaction triggered by medications. Unlike a typical rash, AGEP comes on fast, looks alarming, and demands immediate action. It’s not common - only 1 to 5 people per million get it each year - but when it happens, knowing what to do can make all the difference.
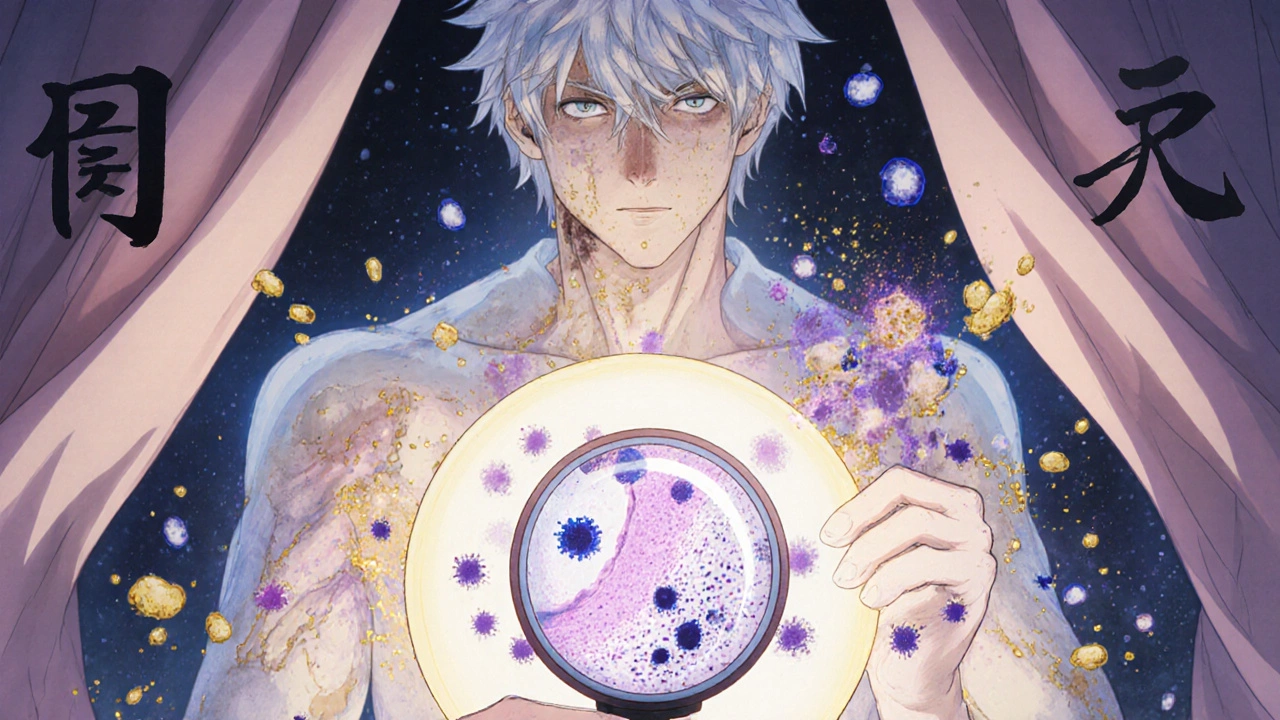
What AGEP Actually Looks Like
AGEP doesn’t start slowly. Within 24 to 48 hours after taking a triggering drug, hundreds of small, sterile pustules - like pinpricks of white pus - appear across the skin. They don’t form around hair follicles. They erupt on red, inflamed patches, often starting in skin folds: under the arms, in the groin, or on the face. Within a day, they spread everywhere. The skin feels hot, tender, and tight. Many people also have a fever above 38.5°C (101.3°F), chills, or feel generally sick.What makes AGEP confusing is how it mimics other conditions. It looks like generalized pustular psoriasis - but it’s not. Psoriasis tends to affect the palms and soles more, and it doesn’t go away so quickly. AGEP clears up in about 10 to 14 days after stopping the drug, with no scarring. The pustules dry up, then the skin peels off like a sunburn. That’s the hallmark: fast in, fast out - if handled right.
What Causes AGEP?
Nearly every case of AGEP is linked to a medication. Antibiotics are the biggest culprits. About 56% of cases are tied to beta-lactams like amoxicillin and amoxicillin-clavulanate. Macrolides like erythromycin come next. Antifungal drugs like fluconazole and calcium channel blockers used for high blood pressure are also common triggers. Even common drugs like paracetamol or ibuprofen can cause it, though rarely.Here’s the twist: the reaction doesn’t always happen right away. Most cases start within 1 to 5 days after taking the drug. But with amoxicillin-clavulanate, it can take up to 14 days. That means people often forget they took the medicine and don’t connect it to the rash. That’s why misdiagnosis is so common - up to 40% of cases in community clinics are wrongly labeled as psoriasis, infection, or heat rash.
Not everyone gets AGEP from these drugs. Genetics may play a role. A specific gene variant, HLA-B*59:01, is linked to higher risk in Asian populations. People with this variant are nearly nine times more likely to develop AGEP after taking certain medications. Research is still ongoing, but this could one day lead to pre-screening tests before prescribing high-risk drugs.
How Doctors Diagnose It
There’s no single blood test for AGEP. Diagnosis is based on three things: the appearance of the rash, the timing after drug exposure, and lab results. Blood tests usually show high white blood cell counts, especially neutrophils - often more than 75% of the total. C-reactive protein (CRP), a marker of inflammation, is almost always elevated.A skin biopsy is the gold standard. Under the microscope, AGEP shows clusters of neutrophils (a type of white blood cell) just below the top layer of skin, with no signs of infection. There’s swelling in the upper dermis and sometimes eosinophils - another clue that it’s a drug reaction, not an infection.
The EuroSCAR group developed a scoring system called the AGEP Probability Score (APS) to help doctors tell it apart from similar conditions. It looks at symptoms, timing, lab results, and biopsy findings. With 94% sensitivity and 89% specificity, it’s become the most reliable tool available. Still, it’s mostly used in specialized centers. In smaller clinics, many doctors rely on experience - and that’s where mistakes happen.
Treatment: Stop the Drug - That’s It?
The single most important step in treating AGEP is stopping the drug that caused it. In over 90% of cases, that’s all you need. The rash will start to fade within a few days and usually clears completely in two weeks. No long-term damage. No scarring. Just supportive care: cool compresses, moisturizers, and antihistamines for itching.But here’s where things get messy. Should you also use steroids?
Some experts say no. Dermatologists from Baylor College of Medicine, based on 15 cases over three years, argue that AGEP is self-limiting - meaning it gets better on its own. Giving systemic steroids like prednisone might mask symptoms, increase infection risk, or even delay recovery. They’ve seen patients do fine without them.
Others say yes - especially if the rash covers more than 20% of the body or if the patient is very sick. A 2023 European study found that patients given oral corticosteroids healed in 7 days on average, compared to 11 days for those who didn’t. Steroids can shorten hospital stays by over three days and reduce complications.
There’s no universal rule. The American Journal of Clinical Dermatology, which surveyed 27 dermatologists across 15 countries, says the decision should be individualized. If you’re young, healthy, and the rash is mild - skip the steroids. If you’re elderly, have diabetes, or the rash is spreading fast - steroids might be worth the risk.
What If Steroids Don’t Work?
In rare cases, AGEP doesn’t respond to stopping the drug or steroids. That’s when newer treatments come in. One of the most promising is secukinumab, a biologic drug normally used for psoriasis. In one case, a patient with AGEP who couldn’t take steroids got secukinumab injections. Within 48 hours, the pustules vanished. Another patient saw complete clearance in 72 hours.Why does this work? AGEP is driven by immune signals - especially IL-17, a protein that tells neutrophils to swarm the skin. Secukinumab blocks IL-17. It’s not FDA-approved for AGEP, but early results are strong. Seven other biologics targeting IL-17 or IL-23 are now in clinical trials. This could change how we treat severe cases in the next few years.
Another option is cyclosporine, an immunosuppressant. It works almost as well as steroids but has fewer side effects like weight gain or blood sugar spikes. It’s used when steroids aren’t safe - for example, in people with kidney disease or uncontrolled hypertension.
When to Go to the Hospital
Most people with mild AGEP can be treated at home. But if you have any of these, go to the ER:- Fever above 38.5°C (101.3°F)
- Pustules covering more than 20% of your skin
- Difficulty swallowing, breathing, or opening your eyes
- Signs of dehydration - dry mouth, dizziness, low urine output
- Confusion or extreme fatigue
Hospital stays average between 5.7 and 9.3 days, depending on severity. In the hospital, you’ll get IV fluids, pain control, and monitoring for infection. Skin care is critical - keeping the skin moist with emollients reduces peeling and discomfort. Patients who get written instructions on moisturizing and sun protection are twice as likely to follow them as those who only get verbal advice.

What Happens After the Rash Clears?
Once the pustules disappear and the skin peels off, you’re not done. You need to avoid the drug that caused it - forever. Even a tiny dose later can trigger a worse reaction. Tell every doctor you see. Write it down in your medical record. If you’re not sure what caused it, see an allergist for patch testing or rechallenge (done only in controlled settings).Long-term, most people recover fully. There’s no increased risk of future skin diseases. But if you’ve had AGEP once, your risk of another drug reaction goes up. That’s why researchers are building a global registry - the RegiSCAR - to track 312 AGEP patients over five years. The goal? To find patterns, improve prevention, and maybe one day predict who’s at risk before they even take the drug.
What’s Changing in AGEP Care?
The field is moving fast. In 2021, the prescribing label for amoxicillin-clavulanate was updated to include AGEP as a known side effect - after 127 confirmed cases were reported to European drug safety databases. The FDA now requires pharmaceutical companies to monitor for AGEP in clinical trials for drugs that affect neutrophils. The European Medicines Agency has similar rules.Next up: a new diagnostic tool called AGEP 2.0, expected in early 2024. It’s more accurate, easier to use in primary care, and includes genetic risk markers. If you’re prescribed a high-risk drug and have Asian ancestry, your doctor might soon ask about your family history of skin reactions.
And biologics? They’re no longer just experimental. Secukinumab and similar drugs are being tested in phase II trials. Early results show 92% of patients respond within days, with no serious side effects. If approved, they could become the go-to treatment for severe or steroid-resistant AGEP - changing a once-ignored condition into a treatable one.
Bottom Line: Don’t Ignore a Sudden Rash
AGEP is rare, but it’s serious. If you develop a sudden, widespread rash with pus-filled bumps after starting a new medication - stop the drug and get medical help immediately. Don’t wait. Don’t assume it’s just an allergy. The faster you identify and remove the trigger, the better your outcome. And if you’ve had it before, make sure every provider knows. Your life might depend on it.Can AGEP be fatal?
Yes, but it’s rare. AGEP has a mortality rate of only 2-4%, much lower than other severe skin reactions like Stevens-Johnson Syndrome, which can kill up to 25% of patients. Death usually happens when complications like infection, dehydration, or organ failure aren’t treated quickly. Most people recover fully with prompt care.
Is AGEP the same as psoriasis?
No. While they look similar, AGEP is triggered by drugs and clears up in weeks. Psoriasis is a chronic autoimmune condition that comes and goes for years. AGEP pustules are sterile and appear suddenly after taking a medication. Psoriasis often affects the scalp, elbows, and knees, and doesn’t resolve so quickly. A skin biopsy can tell them apart.
Can I take the same drug again if the rash went away?
Never. Even if the rash cleared completely, re-exposure to the same drug can cause a much more severe reaction - sometimes fatal. You must avoid that medication for life. Tell all your doctors and pharmacists. Add it to your medical alert bracelet if possible.
How long does it take to recover from AGEP?
Most people start improving within 2-3 days after stopping the drug. The pustules dry up, and the skin begins peeling around day 7-10. Full recovery usually takes 10-14 days. Hospital stays average 5-9 days for moderate to severe cases. No scarring is typical.
Are there any long-term effects of AGEP?
No long-term skin damage occurs in most cases. You won’t develop psoriasis or other chronic conditions because of AGEP. However, your risk of future drug reactions increases. Always report any new rash after taking a medication - even if it seems mild. Keep a list of all drugs that triggered reactions.
Can children get AGEP?
Yes, though it’s rare. Most cases occur in adults, but children and even infants have been diagnosed. The same triggers apply - antibiotics, antifungals, and some painkillers. Children may present with fever and irritability before the rash is obvious. Early recognition is key to prevent complications.
What drugs are most likely to cause AGEP?
The top offenders are antibiotics, especially amoxicillin-clavulanate, erythromycin, and sulfonamides. Antifungals like fluconazole, calcium channel blockers like diltiazem, and even NSAIDs like ibuprofen can trigger it. Over 75% of cases are caused by just these three drug classes. Always ask your doctor if a new prescription is known to cause skin reactions.
Is there a blood test to confirm AGEP?
No single blood test confirms AGEP. But lab results help support the diagnosis: high white blood cell count (especially neutrophils), elevated CRP, and normal liver and kidney function. A skin biopsy is needed to rule out infection or psoriasis. Diagnosis is based on combining symptoms, timing, and lab/biopsy findings - not one test alone.

