The Pharmaceutical Benefits Scheme (PBS) is the backbone of Australia’s healthcare system when it comes to prescription drugs. It’s not just a subsidy program - it’s the reason millions of Australians can afford life-saving medications without going broke. Since 1948, the PBS has ensured that whether you’re a pensioner, a single parent, or a young worker, you pay the same low price for essential medicines. And at the heart of this system? Generics.
How the PBS Works - And Why Generics Matter
The PBS doesn’t give you free medicine. It cuts the cost dramatically. For most people, a prescription that might cost $100 out-of-pocket is reduced to just $31.60. For concession card holders, it’s $7.70. That’s the power of government negotiation. But here’s the key: the PBS doesn’t pay the full price of the brand-name drug. It pays based on the cheapest version available - and that’s almost always a generic. Australia’s reference pricing system, introduced in 2007, forces this. If five drugs treat the same condition, the government sets the subsidy amount based on the lowest-priced one. So if you’re prescribed a brand-name statin, but a generic version exists, the PBS only covers up to the generic’s price. You’d pay the difference if you choose the brand. Most people don’t. That’s why 84% of all prescriptions filled in Australia are for generic medicines by volume. This isn’t just about savings. It’s about scale. In 2024, generic medicines made up $6.2 billion of the $13.5 billion PBS budget. That’s nearly half the total spend - all from drugs that cost a fraction of their branded counterparts.Who Gets What - And Who Gets Left Behind
The PBS covers over 5,400 medicines. That includes everything from insulin and blood pressure pills to antidepressants and cancer drugs. But not all medicines are treated the same. About 42% are restricted - meaning they can only be used for specific conditions. Another 28% need prior approval from Medicare before you can get them. These are often high-cost drugs for rare diseases, chronic conditions, or those with complex dosing. The Highly Specialised Drugs Program (HSDP) handles the most expensive treatments - things like gene therapies or orphan drugs for ultra-rare conditions. But getting listed under HSDP isn’t easy. There are eight strict criteria, including disease severity, life expectancy impact, and cost-effectiveness. Many patients wait years. One 2024 study found that patients with rare diseases often pay over $1,850 out-of-pocket while waiting for PBS approval - money many simply don’t have. And here’s the harsh reality: even with the PBS, cost still stops people. In 2024, 12.3% of general patients - that’s over 1.8 million Australians - admitted to skipping doses or not filling prescriptions because of cost. For those without concession status, five prescriptions a month at $31.60 each adds up to $158. That’s more than some people spend on groceries. Reddit threads from self-funded retirees tell the same story: "I choose between my heart pill and my groceries. Again."Generics vs. Brands - The Real Cost Difference
You might think generics are just cheaper versions of the same drug. They are - but that doesn’t mean they’re the same in the market. By volume, generics make up 84% of prescriptions. By value? Only 22%. Why? Because the price drop after patent expiry is massive. When a new generic enters the market, the price of the original drug often drops by 60% within a year. In cardiovascular drugs, it’s 74%. For antidepressants and antipsychotics, it’s 68%. The top five generic manufacturers - Symbion, Sigma, Mylan, Aspen, and Hospira - control nearly 70% of this market. They compete fiercely on price. And the PBS rewards that competition. The Generic Medicines Pricing Framework, introduced in 2020, speeds this up. After six months, the reference price drops to 60% of the brand’s price. After a year, it’s 43%. That’s a huge incentive for pharmacists to switch patients to generics - and for patients to accept them. But there’s a catch. In biologic therapies - like those for rheumatoid arthritis or Crohn’s disease - generic substitution is still rare. These are complex molecules. Even if a biosimilar exists, doctors are often hesitant to switch. Only 63% of patients on biologics have switched to generics, compared to 95% for statins. The system hasn’t caught up yet.
Why Australia’s System Is Different - And Slower
Compared to the UK’s NICE or Canada’s PMPRB, Australia’s PBS is more flexible but slower. NICE has a hard cap of £20,000-30,000 per quality-adjusted life year (QALY). Australia’s unofficial threshold is AU$50,000 - and even that gets bent for rare diseases. But getting a drug onto the PBS? That’s where the delays kick in. The median time from global launch to PBS listing is 587 days. In Germany, it’s 320. In Canada, 410. That’s almost two years. During that time, patients pay full price. A cancer drug approved by the Therapeutic Goods Administration (TGA) in January might not be on the PBS until November the next year. That’s 14.2 months of out-of-pocket costs - often thousands of dollars. The Pharmaceutical Benefits Advisory Committee (PBAC) reviews every drug. It’s thorough. But it’s also overloaded. The 2024 Productivity Commission found that delays in generic substitution after patent expiry average 217 days. That’s seven months of patients paying more than they should.What’s Changing - And What’s Coming
The government is trying to fix the gaps. The National Health Amendment (Cheaper Medicines) Bill 2025, passed in May 2025, will cut the general patient co-payment from $31.60 to $25.00 starting January 1, 2026. That’s a $6.60 drop per script - $1,584 a year for someone on five prescriptions. The government will cover the cost, but it’s a trade-off: more spending now to reduce hardship later. Budget 2025-26 added $1.2 billion for new PBS listings. Drugs like Talazoparib for prostate cancer and Relugolix for endometriosis are now covered. That’s 150,000 more Australians gaining access. The HSDP is also being reformed. Following a Senate inquiry in 2024, two of the eight criteria for rare disease drugs are being relaxed. That could mean faster access for patients with conditions like Duchenne muscular dystrophy or spinal muscular atrophy. On the tech side, Services Australia is rolling out AI-driven tools to spot inappropriate prescriptions. In 2024, the Auditor-General found $1.2 billion in PBS spending was potentially unnecessary - overprescribing, duplicate scripts, or drugs with no proven benefit. Real-time monitoring could cut that.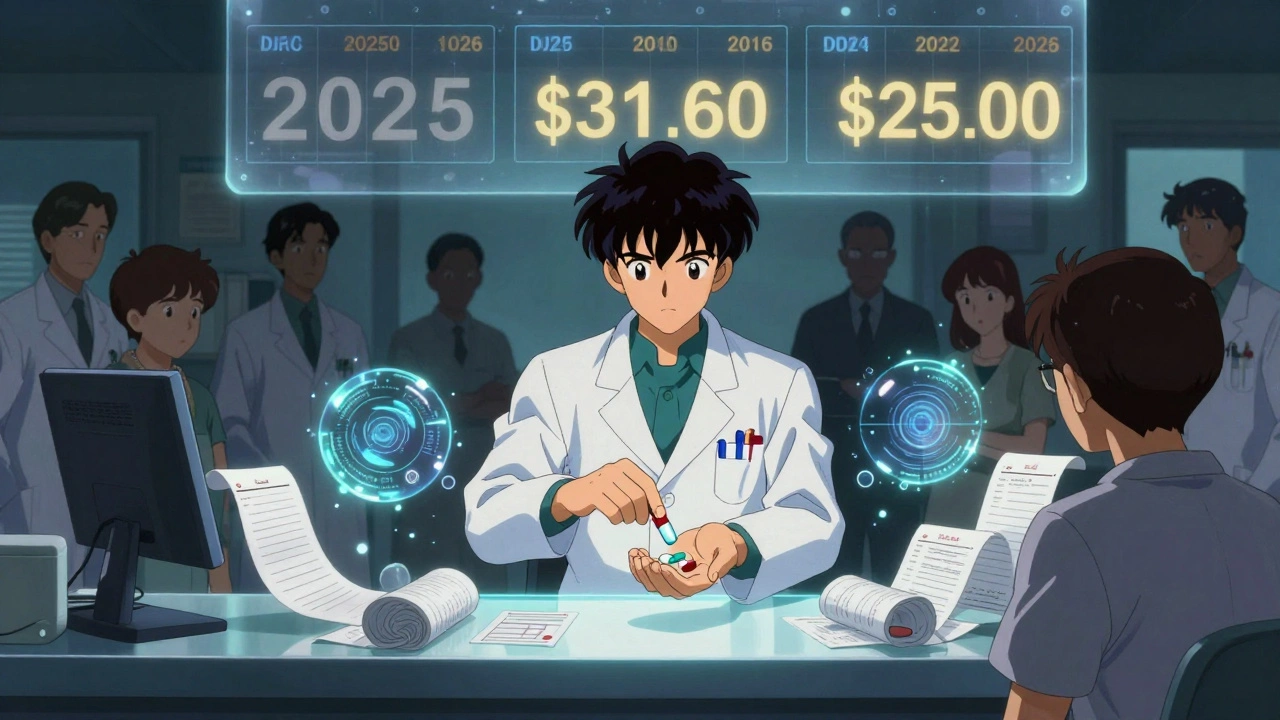
What This Means for You
If you’re on the PBS, you’re part of one of the most efficient public drug systems in the world. You pay less than most other developed countries. You get access to most essential medicines. But it’s not perfect. - If you’re on a concession card: you’re in the best position. Your co-payment is $7.70. Use 60-day scripts to save even more. - If you’re a general patient: the new $25 co-payment in 2026 will help. Track your spending. Once you hit the safety net ($1,571.70 in 2025), your co-payment drops to $31.60 - same as a concession holder. - If you’re on multiple chronic meds: use the PBS app. It tracks your spending, alerts you when you’re near the safety net, and shows you which generics are available. - If you’re waiting for a new drug: ask your doctor about the PBS listing status. If it’s not listed, find out how long it usually takes - and whether there’s a patient assistance program.Where the System Still Fails
The PBS is strong - but it’s not built for everyone equally. Low-income households with multiple chronic conditions are the most vulnerable. A 2025 report found 28% of these families cut back on food to afford their meds. Seventeen percent skip doses. Pharmacists are overwhelmed. They handle an average of 17.3 PBS transactions a day - and nearly 70% say authority-required scripts slow them down. Prescribers need 40 hours of training just to navigate the rules. That’s not a patient issue - it’s a system design flaw. And while generics dominate the market, the system still treats them as second-class. Many patients don’t even know they’re being switched. Pharmacists can substitute without telling you - unless you ask. That’s not transparency. That’s convenience.Final Thoughts
Australia’s PBS is a success story - but it’s also a pressure cooker. It saves billions. It keeps people alive. But it’s strained by aging populations, expensive new drugs, and bureaucratic delays. Generics are the engine that keeps it running. Without them, the system would collapse under the cost of brand-name drugs. The changes coming in 2026 - lower co-payments, faster rare disease access, smarter tech - are steps in the right direction. But real progress will come when the system stops treating patients like numbers and starts treating them like people.What is the PBS co-payment in 2025?
As of July 1, 2024, the PBS co-payment is $31.60 for general patients and $7.70 for concession card holders. These amounts are indexed to the Consumer Price Index each year. In 2025, the co-payment remains at these levels due to a government freeze, even though CPI increases would have raised the general co-payment to $32.80. This freeze saved patients an estimated $127 million in 2025.
How do generic drugs work under the PBS?
Under the PBS, generic drugs are grouped with brand-name versions in "price disclosure groups." The government sets the subsidy amount based on the cheapest drug in the group. Pharmacists can substitute a generic for a brand-name drug unless the doctor marks "Do Not Substitute." Most people choose generics because they cost far less - and the PBS only pays up to the generic’s price. This system drives down costs and has led to 84% of prescriptions being for generics by volume.
Why are some medicines not on the PBS?
Not all medicines are listed on the PBS because they must pass strict evaluations by the Pharmaceutical Benefits Advisory Committee (PBAC). The PBAC looks at clinical effectiveness, cost-effectiveness (using a benchmark of around AU$50,000 per quality-adjusted life year), and budget impact. High-cost drugs, especially for rare diseases, often don’t meet these thresholds or face long delays in approval. Some drugs are also too new - the average time from global launch to PBS listing is nearly two years.
What is the PBS safety net?
The PBS safety net protects people who spend a lot on prescriptions each year. Once you reach the safety net threshold - $1,571.70 for general patients in 2025 - your co-payment drops to $7.70 per script, the same as concession card holders. For concession card holders, the safety net threshold is $316.10, after which they pay only $7.70 per script. This means if you take multiple medications, your out-of-pocket costs eventually become very low.
Can I get generic drugs even if my doctor prescribes a brand name?
Yes, unless your doctor writes "Do Not Substitute" on the prescription. Pharmacists are allowed to switch to a generic version without asking you - and they often do, because it’s cheaper for the PBS and saves you money. If you prefer the brand name, you can ask your pharmacist to dispense it, but you’ll pay the difference between the brand and the generic price.
How do I check if my medicine is on the PBS?
You can check the PBS website, which is updated monthly with new listings. You can also use the Services Australia PBS App, which lets you search for medicines, track your PBS spending, and see when you’re approaching the safety net. If you’re unsure, ask your pharmacist or call the PBS helpline at 1800 020 299. They can confirm whether your medicine is subsidised and what your co-payment will be.

