High cholesterol doesn’t always mean you need to change your diet or start exercising harder. For millions of people, especially those with a history of heart disease or genetic risk, statins are the go-to solution. But what if they don’t work for you? Or worse - what if they make you feel awful? You’re not alone. About 1 in 5 people who start statins stop taking them within a year, often because of muscle pain, fatigue, or just plain frustration. The good news? There are real, science-backed alternatives - and knowing the difference between them can save your heart.
How Statins Actually Work (And Why They’re Still First Choice)
Statins aren’t just another pill. They’re one of the most studied drugs in medical history. Since the 1980s, they’ve been shown to cut the risk of heart attacks and strokes by lowering LDL - the "bad" cholesterol - by up to 50% at the highest doses. Drugs like atorvastatin (Lipitor) and rosuvastatin (Crestor) are the most common. They work by blocking an enzyme in your liver called HMG-CoA reductase. When that enzyme slows down, your liver makes less cholesterol and pulls more LDL out of your blood. The numbers don’t lie. A major analysis of over 39,000 people found that for every 20 mg/dL drop in LDL, your risk of a major heart event drops by 15%. That’s why guidelines from the American Heart Association and the European Society of Cardiology still put statins at the top of the list. They’re cheap, effective, and proven over decades. But here’s the catch: doubling the dose of a statin doesn’t double the benefit. Going from 20 mg to 40 mg of atorvastatin might only drop your LDL another 6%. That’s the law of diminishing returns. And for some people, even low doses cause problems.The Statin Side Effect Problem - And Why It’s Often Overblown
Muscle aches, weakness, or cramps are the most common complaints. About 5-10% of people on statins report them. But here’s what most don’t realize: in clinical trials, up to 80% of those who blame statins for muscle pain actually feel better when they take a placebo instead. That doesn’t mean the pain isn’t real - it just means the link isn’t always what you think. The real danger? Stopping statins without a plan. A study from the American College of Cardiology found that 25% of patients quit statins in the first year - and many of them could’ve stayed on them with a simple switch. Trying a different statin - like switching from simvastatin to pravastatin - can cut side effects dramatically. Simvastatin is processed by the CYP3A4 enzyme, which interacts with grapefruit juice and many other drugs. Pravastatin and rosuvastatin don’t have that problem. Less interaction, fewer side effects. Also, don’t assume you can’t tolerate statins because one made you feel bad. Try another. And if you’re still struggling, talk to your doctor about alternate-day dosing. Some people do just fine taking a statin every other day. It’s not in the package insert, but it’s a real-world trick that works.Ezetimibe: The Quiet Helper
If statins aren’t cutting it - or you can’t take them - ezetimibe (Zetia) is the next step. It doesn’t work like statins. Instead of blocking cholesterol production in the liver, it blocks cholesterol absorption in your gut. Think of it as a bouncer at the door of your intestines, keeping dietary cholesterol from even getting into your bloodstream. Alone, ezetimibe lowers LDL by 15-22%. That’s not as strong as a statin, but it’s not nothing. When you add it to a low-dose statin, the combo can drop LDL another 20-25%. That’s often enough to get someone to their goal without cranking up the statin dose - and that means fewer side effects. Patients on forums like MyHeart.net report that ezetimibe causes far less muscle pain than statins. One user wrote: "Zetia alone got my LDL from 190 to 160, but adding it to my low-dose simvastatin brought it down to 110." That’s the sweet spot: combining two low-risk drugs for a big payoff. And the cost? Generic ezetimibe runs about $10-$15 a month. No insurance hurdles. No injections. Just a small white pill you take once a day. It’s the perfect bridge if statins aren’t working - or if you’re not ready to go bigger.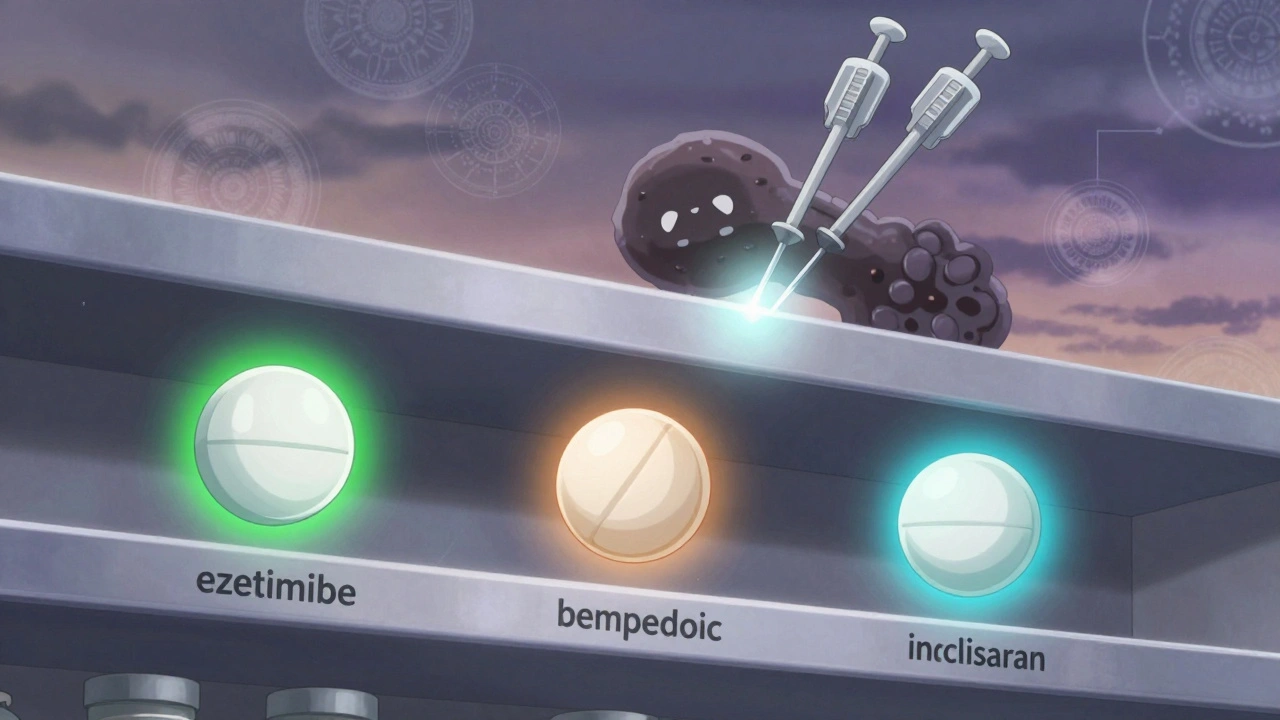
PCSK9 Inhibitors: The High-Tech Option
If you’ve got established heart disease, a family history of early heart attacks, or LDL stuck above 190 despite statins and ezetimibe, it’s time to talk about PCSK9 inhibitors. These are injectable drugs - alirocumab (Praluent) and evolocumab (Repatha) - that came onto the market around 2015. They’re not for everyone. But for some, they’re life-changing. They work by disabling a protein called PCSK9. Normally, PCSK9 tells your liver to destroy LDL receptors. No receptors? No LDL clearance. PCSK9 inhibitors stop that signal, so your liver keeps its receptors and pulls more LDL out of your blood. The result? LDL drops by 50-60%. One Reddit user said, "Repatha lowered my LDL from 220 to 60 in 3 months." That’s not a typo. But here’s what most people don’t know: unlike statins, PCSK9 inhibitors don’t increase the risk of hemorrhagic stroke. In fact, UCLA research found they might be safer for people who’ve had a brain bleed in the past. That’s huge. Statins slightly thin the blood. For someone with a history of brain bleeds, that’s a red flag. PCSK9 inhibitors? No such risk. The downside? Cost and delivery. These shots cost about $5,850 a year. Insurance often denies them unless you’ve tried two statins, ezetimibe, and have a documented reason - like familial hypercholesterolemia or a recent heart attack. One patient spent six months fighting coverage before getting approved. Still, the benefits are clear. Studies show they cut the risk of death from heart disease by 20% in high-risk patients. If you’ve got the right profile and the insurance to back you, this is the most powerful tool outside of surgery.Newer Players: Bempedoic Acid and Inclisiran
The field is evolving fast. Bempedoic acid (Nexletol), approved in 2020, works like a statin but in a different part of the liver. It’s designed for people who can’t tolerate statins. It lowers LDL by about 17% on its own - less than a statin, but with far fewer muscle issues. It’s taken as a pill, once a day. Side effects? Mostly mild: tendon problems in rare cases, and a slight increase in gout. But no muscle pain? That’s a win for many. Then there’s inclisiran (Leqvio), approved in 2021. This is the future. It’s an RNA-based therapy that silences the PCSK9 gene. You get two shots a year - not monthly, not weekly. Just twice a year. When combined with a statin, it drops LDL by 40-50%. It’s not a cure, but it’s the closest thing to a "set it and forget it" cholesterol treatment. The catch? It’s expensive - around $5,000 a year - and access is still limited. But for someone who struggles with daily pills or monthly injections, this is a game-changer.
What About Supplements? Omega-3s, Red Yeast Rice, Plant Sterols?
You’ve seen the ads: "Lower cholesterol naturally with this supplement!" But here’s the truth: none of them come close to statins or the prescription alternatives. Red yeast rice contains a compound similar to lovastatin - but it’s unregulated. One batch might have a safe dose. Another might have toxic levels. The FDA has warned about this. Omega-3s? Great for triglycerides, not LDL. Plant sterols? They can lower LDL by 5-15%, but only if you eat them daily in fortified foods - not a supplement. And they don’t reduce heart attacks. Harvard Health put it bluntly: "If you need to lower your LDL, a statin works, and these supplements do not." That’s not hype. That’s data from clinical trials. Supplements can support heart health - but they’re not substitutes for proven medication.How to Decide What’s Right for You
There’s no one-size-fits-all. Here’s how to think about it:- First, try a statin. Start low. Give it 6-8 weeks. Get your LDL checked. If it’s working and you feel fine - stick with it.
- If you have side effects, don’t quit. Switch statins. Try pravastatin or rosuvastatin. Ask about alternate-day dosing.
- If you still can’t tolerate statins, add ezetimibe. It’s safe, cheap, and effective as a combo.
- If you have heart disease and LDL is still too high, talk to your doctor about PCSK9 inhibitors. Insurance may require paperwork, but it’s worth it.
- If you hate pills or shots, ask about inclisiran. Two shots a year? That’s easier than daily medication.
What’s Next? The Future of Cholesterol Treatment
Scientists are already working on oral versions of PCSK9 inhibitors - no needles needed. Gene editing therapies are in early trials. One day, we might fix the PCSK9 gene with a single treatment. But for now, the tools we have work. The biggest barrier isn’t science. It’s access. Statins cost $4 a month. PCSK9 inhibitors cost over $5,000. That’s why so many people never get the care they need. If you’re struggling to afford treatment, ask about patient assistance programs. Drugmakers have them. Nonprofits have them. Don’t give up because of cost. Your heart doesn’t care about your insurance plan. It only cares about whether your LDL is under control.Can I stop taking statins if I feel better?
No. Statins work as long as you take them. Stopping them - even if your cholesterol looks good - lets LDL rise again, and your risk of heart attack or stroke goes back up. If you want to stop, talk to your doctor first. They may lower your dose, switch you to a different drug, or add ezetimibe to help you taper safely.
Do statins cause diabetes?
Yes, but the risk is small. Studies show statins slightly increase the chance of developing type 2 diabetes - about 1 in 250 people over 4 years. But for every one person who develops diabetes, about 5 heart attacks or strokes are prevented. If you’re at risk for diabetes, your doctor will monitor your blood sugar. The benefits still outweigh the risk for most people.
Are PCSK9 inhibitors safe for long-term use?
Yes. Clinical trials have followed patients on PCSK9 inhibitors for over 5 years, with no major safety concerns. They don’t damage the liver or muscles like statins can. The main side effects are mild injection-site reactions and occasional cold-like symptoms. Long-term data is still being collected, but so far, they’re among the safest cholesterol drugs available.
Why don’t doctors always suggest PCSK9 inhibitors first?
Cost and guidelines. Statins are proven, cheap, and effective for most people. PCSK9 inhibitors are reserved for high-risk patients who haven’t reached their LDL goal with statins and ezetimibe. Insurance companies require you to try cheaper options first. But if you have familial hypercholesterolemia, heart disease, or LDL over 190 despite meds, you’re a strong candidate - even if your doctor doesn’t bring it up first.
What’s the best way to monitor my cholesterol on these meds?
Get a lipid panel 4-12 weeks after starting or changing any cholesterol medication. That’s when levels stabilize. After that, check every 6-12 months unless your doctor says otherwise. Don’t rely on how you feel - LDL doesn’t cause symptoms. Only blood tests show if you’re on track.

