Every year, millions of Americans take herbal supplements thinking they’re harmless because they’re "natural." But what if that ginkgo pill you’re taking to boost memory is quietly making your blood thinner work too well? Or what if the St. John’s wort you use for low mood is canceling out your birth control or your heart medication? The truth is, herbal supplements aren’t harmless snacks-they’re powerful substances that can interact with prescription drugs in ways that are dangerous, even deadly.
Why Herbal Supplements Aren’t Always Safe
People assume that if something comes from a plant, it’s safe. That’s a myth. Herbs contain active chemicals-sometimes dozens of them-that can change how your body handles medications. These aren’t just minor tweaks. They can make drugs stop working entirely, or turn them into toxic doses. Take St. John’s wort, for example. It’s one of the most popular herbal mood boosters in the U.S. But it’s also the most dangerous when mixed with other drugs. It speeds up the liver’s ability to break down medications by turning on a key enzyme called CYP3A4. That enzyme processes about half of all prescription drugs. When St. John’s wort activates it, your body flushes out drugs like cyclosporine (used after organ transplants), HIV medications, birth control pills, and even digoxin (for heart rhythm) before they can do their job. Studies show cyclosporine levels can drop by 57%-enough to trigger organ rejection. Birth control failure? There are documented cases of pregnancy in women taking St. John’s wort alongside pills. And it’s not just St. John’s wort. Garlic, ginkgo, goldenseal, and danshen all have proven, serious interactions. Garlic reduces the blood levels of saquinavir, an HIV drug, by over half. Ginkgo can double the bleeding risk when taken with warfarin. Danshen, often used for heart health, increases the chance of irregular heartbeat when combined with digoxin. These aren’t theoretical risks. They’re documented in clinical studies, hospital reports, and patient stories.How These Interactions Actually Happen
There are two main ways herbs mess with medications: pharmacokinetic and pharmacodynamic. Pharmacokinetic means the herb changes how your body absorbs, moves, or gets rid of the drug. Most often, this happens through the liver’s cytochrome P450 enzymes-especially CYP3A4, CYP2C9, and CYP2C19. Some herbs, like St. John’s wort and garlic, force these enzymes to work faster, clearing drugs too quickly. Others, like goldenseal and black cohosh, block them, causing drugs to build up to dangerous levels. One study found goldenseal increased dextromethorphan (a common cough medicine) levels by 30-50%, raising the risk of serotonin syndrome-a potentially fatal condition. Then there’s pharmacodynamic interaction: the herb and the drug have similar effects, and together they amplify each other. Ginseng, for instance, has vitamin K-like properties that can weaken warfarin’s blood-thinning effect. In one case, a patient’s INR (a measure of blood clotting) dropped from 4.9 to 1.9 after starting ginseng-meaning their blood was clotting too fast. Danshen does the opposite: it prevents blood platelets from sticking together, making bleeding more likely when paired with aspirin, clopidogrel, or warfarin. Even something as simple as hawthorn-a supplement many take for mild high blood pressure-can drop systolic pressure another 10-15 mmHg when combined with beta-blockers. One patient ended up in the ER with a blood pressure of 85/50 after taking hawthorn with lisinopril.The Most Dangerous Herbal Supplements
Not all herbs are equal in risk. Some are relatively safe. Others? They’re ticking time bombs.- St. John’s wort: The #1 offender. Interacts with at least 15 drug classes. Can cause transplant rejection, birth control failure, antidepressant withdrawal, and loss of seizure control.
- Ginkgo biloba: Increases bleeding risk with warfarin, aspirin, and NSAIDs. Linked to multiple bleeding incidents in patients on anticoagulants.
- Goldenseal: Blocks liver enzymes, raising levels of metoprolol, dextromethorphan, and many others. Risk of overdose is real.
- Danshen: Increases bleeding and can trigger irregular heartbeat with digoxin. A 2023 Mayo Clinic alert specifically warned about this combo.
- Garlic: Lowers levels of HIV drugs and some statins. Can also increase bleeding risk.
- Ginseng: Reduces warfarin effectiveness. May interfere with blood pressure meds and insulin.
Why Doctors Don’t Always Know
You might think your doctor would catch this. But they often don’t. In a 2016 study of 299 hospitalized patients, 25% were taking herbal supplements-but doctors missed it in 72% of cases. Why? Because they don’t ask. Most intake forms just say, "Are you taking any supplements?" That’s too vague. Patients think "supplements" means vitamins and calcium. They don’t think of turmeric tea, elderberry syrup, or kava root. One study found that when doctors specifically asked, "Do you drink herbal teas or take any botanicals?"-they caught 35% more users. And even when patients do mention them, many providers don’t know the science. A 2022 assessment showed that 62% of clinicians missed the interaction between American ginseng and warfarin. Pharmacists spend an average of 12 minutes counseling patients on herb-drug risks-but for St. John’s wort? It takes 18 minutes. Most clinics don’t have that kind of time.What You Should Do
If you’re taking any prescription medication-especially for heart disease, blood thinning, epilepsy, HIV, cancer, or mental health-here’s what you need to do:- Make a list. Write down every herb, tea, tincture, or capsule you take-even if you think it’s "just for relaxation" or "natural." Include turmeric, ginger, chamomile, and green tea extracts.
- Bring it to every appointment. Don’t wait for your doctor to ask. Hand them the list. Say, "I’m taking these herbs. Are they safe with my meds?"
- Check high-risk combos. If you’re on warfarin, digoxin, cyclosporine, birth control, or HIV meds, avoid St. John’s wort, ginkgo, goldenseal, garlic, and danshen unless your doctor says it’s okay.
- Watch for warning signs. Unexplained bruising, dizziness, irregular heartbeat, sudden changes in mood or energy, or worsening symptoms could mean an interaction is happening.
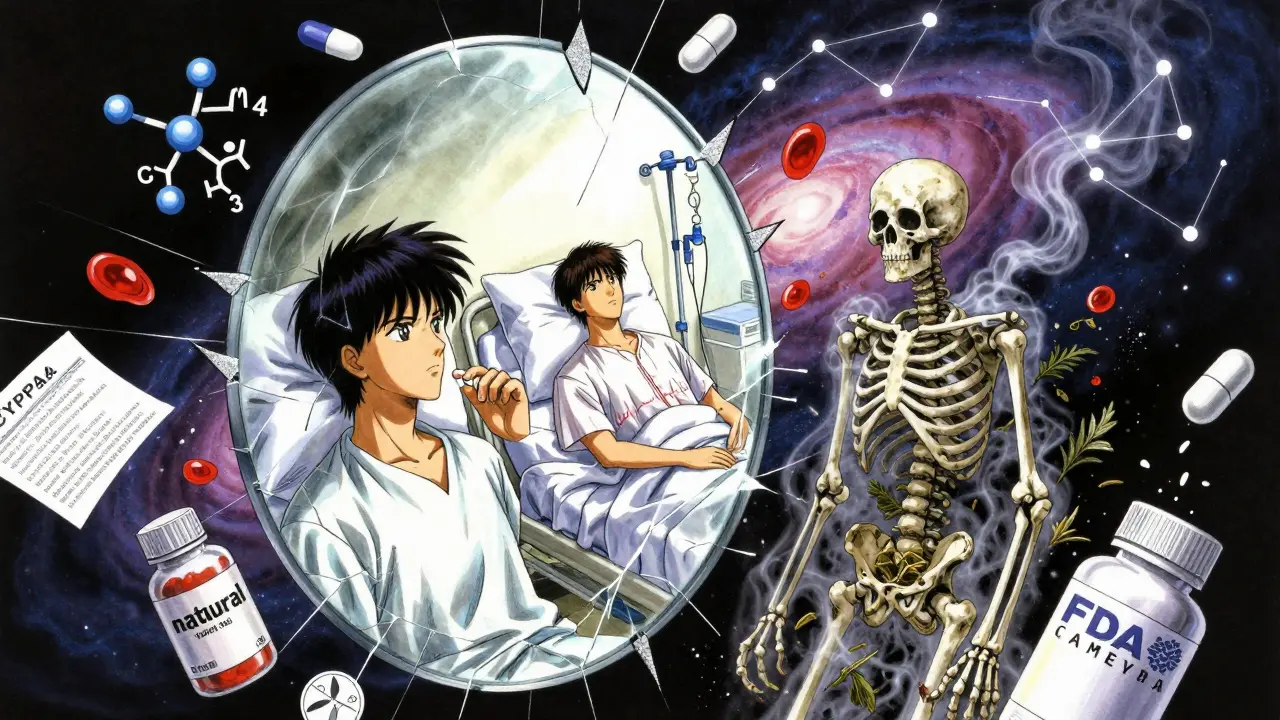
The Bigger Problem: Lack of Regulation
Here’s the scary part: herbal supplements aren’t held to the same standards as drugs. Under the 1994 Dietary Supplement Health and Education Act (DSHEA), manufacturers don’t have to prove safety or interactions before selling. The FDA can only act after harm is done-and even then, they issue only about 12 warning letters a year for interaction risks, despite over 80,000 products on the market. Only 15% of supplement labels include interaction warnings. And 77% of users believe herbal products are safer than prescription drugs-even though 62% of them take both. That disconnect is deadly. New efforts are underway. The FDA released draft guidance in 2023 pushing for mandatory interaction testing. The European Medicines Agency now requires it for herbal medicines. The NIH spent $12.7 million in 2023 just to study herb-drug interactions. And AI tools like the Herb-Drug Interaction Prediction Engine are now predicting new risks with 87% accuracy. But until those rules are enforced, the burden falls on you.Final Word: Natural Doesn’t Mean Harmless
Herbal supplements are not benign. They’re bioactive compounds with real, measurable effects on your body’s chemistry. What makes them dangerous isn’t the fact that they’re natural-it’s that we treat them like they are. If you’re on medication, your herbal supplement isn’t just a side note. It’s part of your drug regimen. And just like mixing two pills can be risky, mixing a pill and a plant can be just as dangerous-sometimes more so, because no one’s tracking it. Talk to your doctor. Show them your list. Ask the hard questions. Your life might depend on it.Can herbal supplements really interfere with prescription drugs?
Yes. Herbs like St. John’s wort, ginkgo, goldenseal, and danshen can alter how your body processes medications. They can make drugs less effective, increase their toxicity, or cause dangerous side effects like bleeding, irregular heartbeat, or organ rejection. These aren’t rare or theoretical-they’re documented in clinical studies and real patient cases.
Which herbal supplements are the most dangerous with medications?
St. John’s wort is the most dangerous, with over 15 known drug interactions, including with birth control, HIV meds, and transplant drugs. Ginkgo increases bleeding risk with blood thinners. Goldenseal can cause toxic buildup of drugs like metoprolol and dextromethorphan. Danshen raises the risk of irregular heartbeat when taken with digoxin. Garlic and ginseng also interfere with several common medications.
Why don’t my doctors know about these interactions?
Most doctors don’t ask about herbal supplements because they’re not trained to. Patients often don’t mention them, thinking they’re harmless or not "real" medicine. Studies show up to 72% of patients taking herbs aren’t disclosed to their providers. Even when they are, many clinicians lack the training to recognize the risks.
Are herbal supplements regulated like drugs?
No. Under the 1994 DSHEA law, supplement makers don’t need FDA approval before selling. They don’t have to prove safety, purity, or interaction risks. The FDA can only act after harm occurs-and they issue very few warnings. Only 15% of supplement labels include interaction warnings, even though most users take them with prescription drugs.
What should I do if I’m already taking herbs and medications?
Stop taking the herbs until you talk to your doctor or pharmacist. Make a complete list of everything you take-teas, tinctures, capsules, even ginger or turmeric. Bring it to your next appointment and ask, "Are these safe with my current medications?" Don’t rely on labels or internet advice. If you’re on blood thinners, heart meds, HIV drugs, or birth control, be especially cautious.

