Antihypertensive Medication & Gout Risk Comparison Tool
Select Your Medication
Medication Impact Analysis
Lifestyle Recommendations
Stay hydrated (2-3 liters of water daily), limit high-purine foods, maintain healthy weight, and monitor uric acid levels regularly.
When you hear Labetalol is a non‑selective beta blocker used to treat high blood pressure and certain heart conditions, you probably think about heart health, not joint pain. Yet many patients ask whether gout - a painful arthritis triggered by uric acid crystals - could be linked to this medication.
Quick Takeaways
- Labetalol primarily affects beta‑adrenergic receptors; it does not directly raise uric acid levels.
- Evidence of a strong link between labetalol and gout is limited and mostly anecdotal.
- Other antihypertensives, especially diuretics, have a clearer connection to gout.
- If you notice joint pain after starting labetalol, talk to your doctor - it could be a coincidence or a drug interaction.
- Lifestyle tweaks (hydration, diet, weight control) often do more for gout risk than switching the blood‑pressure pill.
How Labetalol Works
Labetalol blocks both beta‑1 and beta‑2 receptors, slowing heart rate and relaxing blood vessels. It also has weak alpha‑blocking activity, which helps lower peripheral resistance. By reducing the heart’s workload, it keeps blood pressure in check without heavily influencing kidney excretion of uric acid.
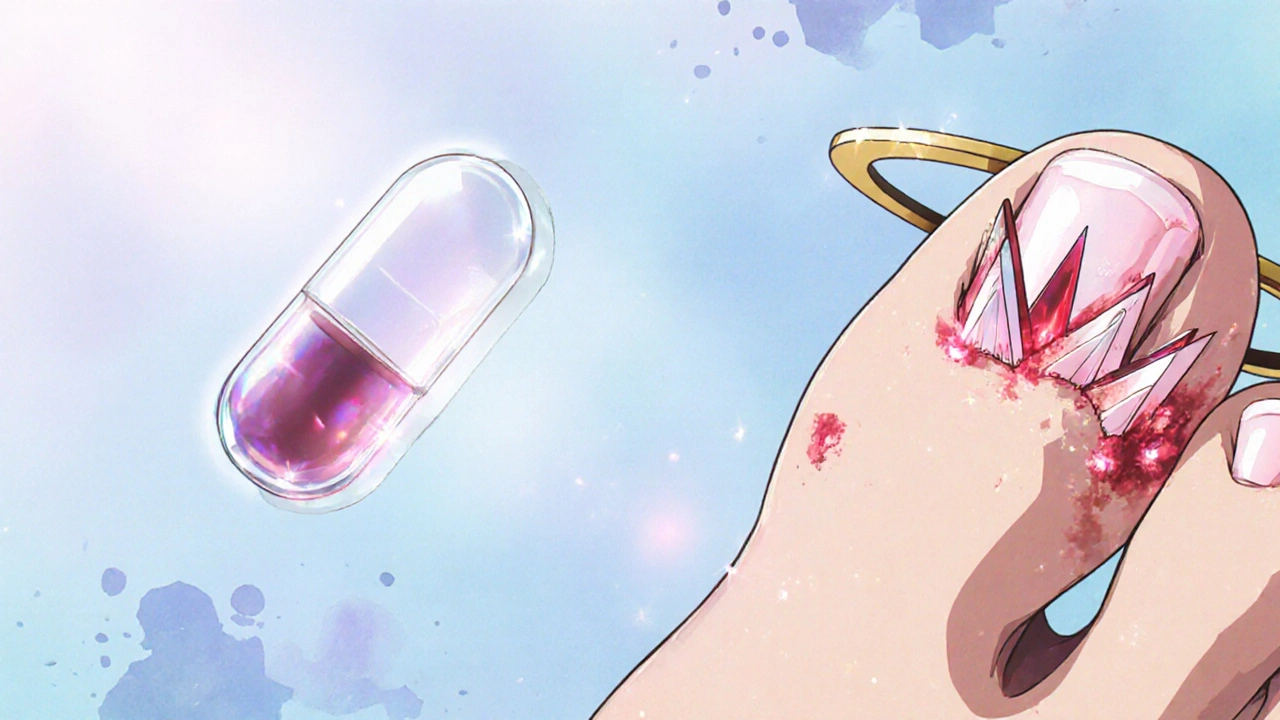
What Is Gout?
Gout occurs when uric acid, a waste product of purine metabolism, builds up in the bloodstream and forms sharp crystals in joints. The big toe is a classic spot, but any joint can flare up. Typical triggers include high‑purine foods (red meat, seafood), alcohol, dehydration, and certain medicines that slow uric‑acid clearance.
Does Labetalol Raise Uric Acid?
Most clinical studies focus on diuretics (like thiazides) and low‑dose aspirin as culprits for raising serum uric acid. Labetalol isn’t listed among the usual suspects. A handful of case reports have noted gout flares shortly after starting labetalol, but these are isolated and often involve other risk factors - such as pre‑existing hyperuricemia, obesity, or concurrent use of uric‑acid‑raising drugs.
One 2022 retrospective analysis of 1,800 hypertensive patients found no statistically significant difference in uric‑acid levels between those on labetalol and those on other beta blockers. The average serum uric acid stayed around 5.8 mg/dL, well below the gout threshold of 7.0 mg/dL for men.

Key Factors That Can Influence Gout Risk While on Labetalol
- Kidney Function: If your kidneys aren’t filtering well, any drug can indirectly affect uric‑acid handling.
- Concurrent Medications: Combining labetalol with a thiazide diuretic, low‑dose aspirin, or cyclosporine can raise uric acid.
- Diet and Hydration: A diet high in purines or low fluid intake can tip the balance.
- Weight and Metabolic Health: Obesity and insulin resistance both raise uric‑acid production.
Managing Gout If You’re Taking Labetalol
Even if labetalol isn’t the main problem, you can still keep gout at bay.
- Stay Hydrated: Aim for at least 2‑3 liters of water daily to help flush uric acid.
- Watch Purine‑Rich Foods: Limit organ meats, anchovies, and sugary drinks.
- Control Alcohol: Beer and spirits can spike uric acid; keep consumption modest.
- Maintain a Healthy Weight: Losing even 5 % of body weight can lower uric‑acid levels.
- Monitor Serum Uric Acid: Have your doctor check it every 3‑6 months, especially after a medication change.
- Use Acute Gout Meds Wisely: NSAIDs, colchicine, or low‑dose steroids can treat flares. Talk to your doctor before mixing them with labetalol.
Comparing Antihypertensives for Gout Risk
| Medication Class | Typical Effect on Serum Uric Acid | Gout‑Friendly? | Common Use Cases |
|---|---|---|---|
| Labetalol (beta‑blocker + alpha‑blocker) | Neutral - no significant change | Generally safe | Hypertension, hypertensive emergencies |
| Thiazide Diuretics | Increase uric acid (0.3‑0.7 mg/dL) | Not ideal for gout patients | First‑line hypertension |
| ACE Inhibitors (e.g., lisinopril) | Neutral or slight decrease | Gout‑friendly | Hypertension, heart failure |
| ARBs (e.g., losartan) | Often lowers uric acid | Very gout‑friendly | Hypertension, diabetic nephropathy |
| Calcium Channel Blockers | Neutral | Gout‑friendly | Hypertension, angina |
When to Talk to Your Doctor
If you notice any of the following after starting labetalol, schedule a check‑up:
- Sudden joint pain, especially in the big toe
- Swelling or redness that lasts more than a day
- Kidney‑related symptoms (e.g., foamy urine, swelling of ankles)
- Unexplained changes in blood pressure control
Most of the time, the doctor will run a simple blood test for serum uric acid and may adjust your medication regimen if needed. Switching to an ARB like losartan is a common strategy when gout becomes a concern.
Bottom Line
There isn’t strong scientific proof that Labetalol and gout are directly linked. The drug itself is largely neutral regarding uric‑acid levels. However, individual health factors, other medicines, and lifestyle choices can create the impression of a connection. Staying hydrated, watching diet, and regular lab checks are the best ways to keep both blood pressure and gout under control.
Frequently Asked Questions
Can labetalol cause a gout flare?
Current research shows no clear causal relationship. If a flare occurs, it’s more likely linked to other risk factors like diet, kidney function, or concurrent diuretic use.
Are there antihypertensives that actually lower uric acid?
Yes. Losartan (an ARB) and some calcium‑channel blockers have been shown to modestly reduce serum uric‑acid levels, making them good choices for patients with gout.
What lifestyle steps help prevent gout while on blood‑pressure meds?
Drink plenty of water, limit high‑purine foods (red meat, shellfish), reduce alcohol, maintain a healthy weight, and keep regular check‑ups for uric‑acid levels.
Should I stop labetalol if I develop gout?
Don’t stop the medication on your own. Discuss options with your doctor; they may switch you to an ARB or adjust other meds that affect uric acid.
How often should I have my uric‑acid level checked?
If you have gout or high risk, every 3‑6 months is reasonable. Otherwise, an annual check‑up alongside routine labs is sufficient.