Medication Side Effect Checker
Check Your Medication Risk
Find out how common sexual side effects are for your medication and see lower-risk alternatives.
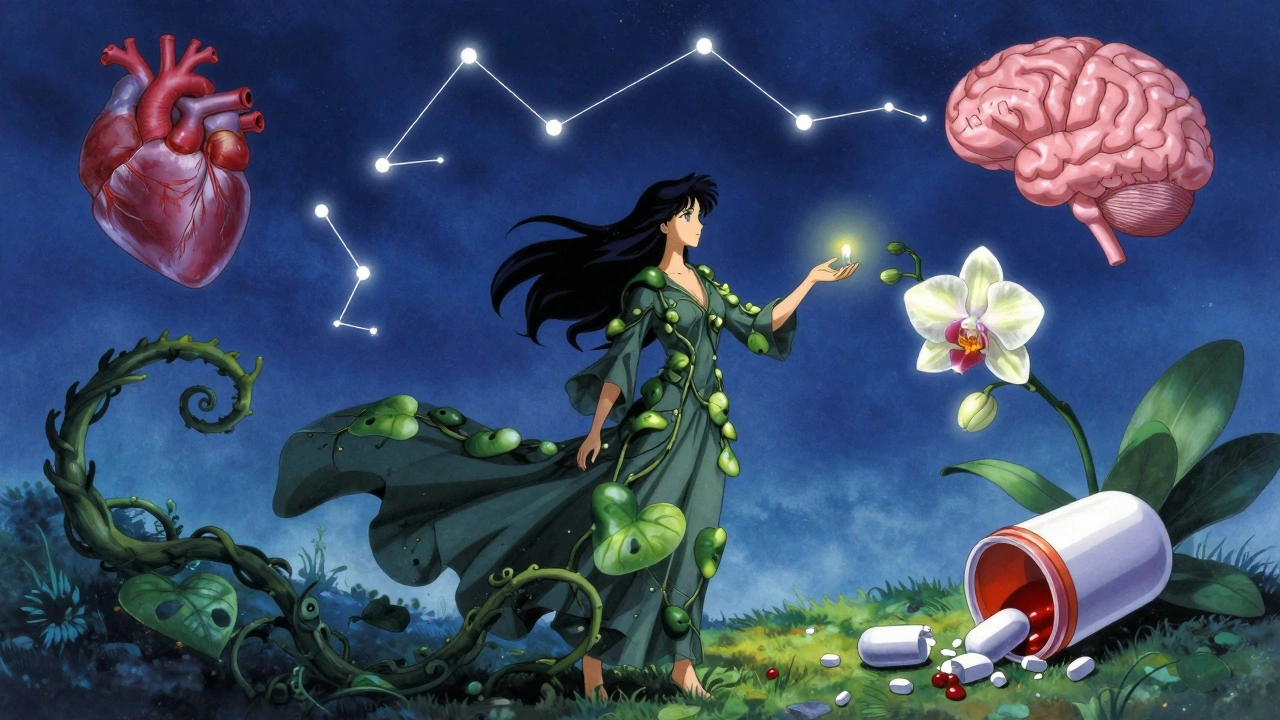
It’s not rare to hear someone say, "I’m taking this pill for my depression, but it’s killing my sex life." And they’re not alone. Up to 73% of people on certain antidepressants report sexual side effects - lowered desire, trouble getting or keeping an erection, delayed or absent orgasm, or even numbness in the genitals. These aren’t rare glitches. They’re common, well-documented, and often ignored by doctors and patients alike.
Why This Happens
Many medications affect sexual function because they change brain chemistry, hormone levels, or blood flow. The brain controls desire, arousal, and orgasm through neurotransmitters like serotonin, dopamine, and norepinephrine. When a drug alters these chemicals - even to help with depression, high blood pressure, or prostate issues - it can accidentally shut down sexual response. For example, SSRIs like Prozac, a selective serotonin reuptake inhibitor used to treat depression and anxiety and Zoloft, another SSRI commonly prescribed for depression and OCD increase serotonin in the brain. That helps mood - but too much serotonin can dampen libido and make it harder to reach orgasm. It’s like turning up the volume on one channel while muting the rest.Antidepressants: The Biggest Culprits
Antidepressants are the most common cause of drug-induced sexual problems. Among them, not all are equal.- Paroxetine (Paxil), an SSRI with the highest risk of sexual side effects affects up to 65% of users - the highest of any antidepressant.
- Fluvoxamine (Luvox), an SSRI used for OCD and anxiety hits around 59%.
- Sertraline (Zoloft), one of the most prescribed SSRIs affects about 56%.
- Fluoxetine (Prozac), a long-acting SSRI is close behind at 54%.
Heart Medications: More Than Just Blood Pressure
High blood pressure drugs are another major source of sexual problems. About 10% of heart failure patients say their meds are the reason they’ve lost interest in sex.- Hydrochlorothiazide (Microzide), a thiazide diuretic used to lower blood pressure is the most common cause of erectile dysfunction among antihypertensives.
- Beta blockers, medications like atenolol and metoprolol that slow heart rate also reduce blood flow and lower libido.
- Spironolactone (Aldactone), a potassium-sparing diuretic used for heart failure and acne can cause breast enlargement and reduced desire in men.

Prostate and Hormone Drugs
Men taking 5-alpha reductase inhibitors, medications like finasteride and dutasteride used for enlarged prostate or hair loss often face sexual side effects. About 6-16% report lower libido, 5-9% get erectile dysfunction, and up to 21% have problems with ejaculation. These drugs block dihydrotestosterone (DHT), a hormone tied to sexual function. Lower DHT = less drive, harder erections, and sometimes dry orgasms. The effects can linger even after stopping the drug. For men with prostate cancer, Antiandrogens, drugs like bicalutamide that block testosterone are used to starve cancer cells. But they almost always cause complete loss of libido, erectile dysfunction, and sometimes breast growth. These aren’t side effects - they’re the intended outcome. Still, counseling before treatment helps men adjust better.Other Surprising Offenders
Some medications you might not expect also mess with sex:- Gabapentin and Pregabalin, antiseizure drugs also used for nerve pain can lower free testosterone and cause erectile dysfunction. Studies link them to increased sex hormone binding globulin, which locks up testosterone so your body can’t use it.
- Opioids, painkillers like oxycodone and hydrocodone disrupt the hypothalamic-pituitary-gonadal axis. This leads to low testosterone, low libido, and erectile problems - even in younger men.
- Proton pump inhibitors, heartburn drugs like omeprazole and esomeprazole have been tied to reduced libido and ED in some users, though the mechanism isn’t fully clear.
What Can You Do?
Never stop a medication cold turkey. Withdrawal from antidepressants or blood pressure drugs can be dangerous. But you don’t have to live with a broken sex life. Here’s what works:- Switch meds. Talk to your doctor about switching from paroxetine to bupropion, or from a beta blocker to valsartan. Many people feel better within weeks.
- Adjust the dose. Sometimes lowering the dose reduces side effects without losing the benefit.
- Try a "drug holiday." For SSRIs, skipping the pill for a day or two (under medical supervision) can restore sexual function temporarily. Some men take their pill after sex instead of before.
- Add a helper. For SSRI-induced erectile dysfunction, Sildenafil (Viagra), a PDE5 inhibitor used to treat ED works in 74-95% of cases.
- Move more. Exercise boosts blood flow, improves mood, and raises testosterone. Even 30 minutes of walking daily can help.
When to Speak Up
If you’ve noticed changes in your sex life after starting a new medication - whether it’s low desire, trouble with arousal, or delayed orgasm - tell your doctor. Don’t wait. Don’t assume it’s "just stress" or "getting older." Many doctors don’t bring it up. But you should. Ask: "Could this medication be affecting my sex life? Are there alternatives?" If they brush you off, find someone who listens.The Bigger Picture
Sexual health isn’t a luxury. It’s part of overall well-being. Losing it can lead to depression, relationship strain, and quitting treatment - which is worse than the side effects. Newer antidepressants and heart meds are being designed with sexual side effects in mind. The FDA now requires drug makers to track sexual function in trials. Research is uncovering why some people are more sensitive than others - possibly due to genetics. Until then, knowledge is power. Knowing which drugs cause what, and what to do about it, puts you in control.Can antidepressants cause permanent sexual side effects?
In most cases, sexual side effects from antidepressants go away after stopping the medication. But for a small number of people - especially those on SSRIs long-term - symptoms like low libido or trouble with orgasm can persist for months or even years after discontinuation. This is called Post-SSRI Sexual Dysfunction (PSSD), and while rare, it’s real. If you experience lasting issues, consult a specialist in sexual medicine.
Do all SSRIs cause the same level of sexual problems?
No. SSRIs vary widely. Paroxetine has the highest risk - up to 65% of users report sexual side effects. Fluoxetine and sertraline are close behind at 54% and 56%. But escitalopram (Lexapro) and citalopram (Celexa) tend to have slightly lower rates. Bupropion and mirtazapine, while not SSRIs, are often chosen specifically because they don’t cause these issues. Your doctor can match the drug to your priorities.
Can blood pressure meds cause low libido in women?
Yes. Studies show that up to 41% of women on antihypertensives report decreased sexual desire, and 34% say they experience less pleasure during sex. Thiazide diuretics like hydrochlorothiazide and beta blockers are the biggest culprits. Angiotensin II receptor blockers like valsartan, however, have been linked to improved sexual fantasies and desire in women. If you’re a woman on blood pressure meds and noticing changes, ask about switching.
Is it safe to take Viagra with antidepressants?
Yes, in most cases. Sildenafil (Viagra) and other PDE5 inhibitors like tadalafil (Cialis) are commonly used to treat erectile dysfunction caused by SSRIs. Studies show they work in 74-95% of these cases. But always check with your doctor first - combining them with certain heart meds or nitrates can be dangerous. Your doctor can help you find the right dose and timing.
What should I do if my doctor dismisses my concerns?
If your doctor ignores your concerns, it’s time to find a new one. Sexual health matters. There are specialists - urologists, psychiatrists, and sexual medicine clinicians - who are trained to handle this. Bring printed data from reputable sources like the Mayo Clinic or peer-reviewed studies. You’re not being dramatic; you’re advocating for your quality of life. Don’t settle for a doctor who doesn’t listen.
Can exercise help reverse medication-induced sexual side effects?
Yes. Regular physical activity improves blood flow, increases testosterone, and reduces stress - all of which help sexual function. Even moderate walking 3-5 times a week has been shown to improve libido and erectile quality in men on antidepressants and beta blockers. For women, exercise can boost arousal and reduce the emotional impact of low desire. It’s not a cure, but it’s one of the few interventions that helps without adding more pills.

