When you have a sore knee or aching shoulder, you might reach for a cream or gel. Or maybe you grab a pill. Both seem to target pain, but they work in very different ways-and the difference matters more than you think. One goes straight to the spot. The other floods your whole body. And that’s where safety, effectiveness, and side effects come into play.
How Your Body Handles Topical vs. Oral Medications
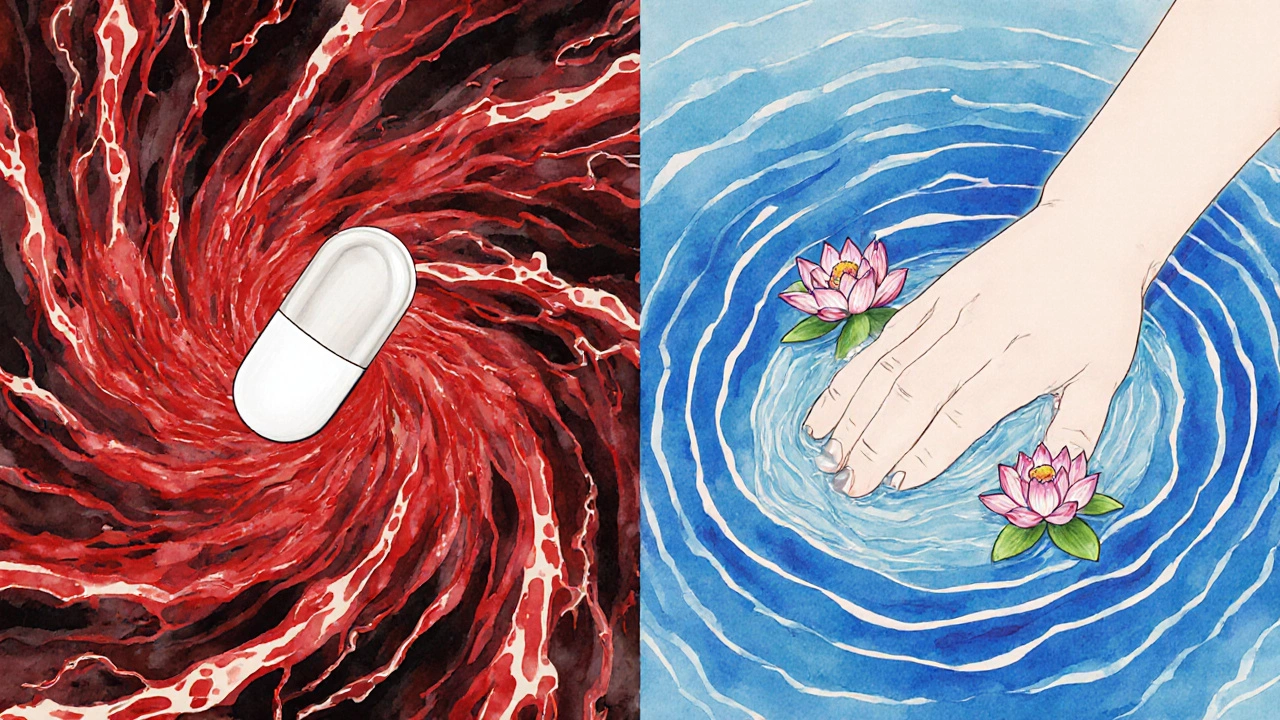
Topical medications-like gels, creams, or patches-are meant to stay local. You put them on your skin, and they’re designed to work right where you apply them. Oral meds, on the other hand, are swallowed. They travel through your stomach and intestines, get absorbed into your bloodstream, and then circulate everywhere. That’s the core difference: topical = targeted. oral = full-body.
Here’s what happens behind the scenes. When you rub on a topical NSAID like diclofenac gel, only a tiny fraction-less than 5%-actually gets into your blood. The rest stays in your skin and muscles near the pain. That’s why you can treat a swollen knee without worrying about your stomach. Oral NSAIDs? They’re built to absorb well. About 70-90% of the dose enters your bloodstream. That’s great if you need pain relief all over, but it also means your liver, kidneys, and gut are dealing with the full drug load.
Even more surprising: some topical products, like fentanyl patches, are engineered to bypass the skin barrier entirely. These transdermal systems use special chemicals to push drugs deeper, delivering steady doses over days. But most over-the-counter creams? They barely make it past the top layers of skin.
Why Systemic Absorption Matters for Safety
Systemic absorption isn’t just a technical term-it’s the reason one drug can save your stomach and another can wreck it.
Oral NSAIDs are linked to serious gastrointestinal problems. Studies show 15% of people who take them regularly develop ulcers, bleeding, or severe indigestion. The FDA reports over 18,000 hospitalizations each year in the U.S. just from these complications. Why? Because NSAIDs block protective enzymes in the stomach lining. The higher the dose, the worse it gets. And for older adults? The risk spikes.
Topical NSAIDs? The numbers flip. Less than 1% of users report stomach issues. The same 2023 Arthritis Foundation survey found 89.7% of patients preferred topical versions-not because they worked better, but because they didn’t cause acid reflux, nausea, or bloating. The FDA’s adverse event database shows 14.7 serious incidents per 10,000 oral NSAID prescriptions. For topical? Just 1.2.
But here’s the catch: topical doesn’t mean zero absorption. If you apply a large amount over a wide area-say, your entire back-or if your skin is broken, dry, or thin (common in older adults), more drug can get through. One case study showed a patient using diclofenac cream on 30% of their body had blood levels high enough to cause liver stress. So “localized” doesn’t mean “safe if you misuse it.”
Real-World Efficacy: Do Topical Meds Actually Work?
People often assume topical meds are weaker. That’s not always true.
For localized pain-like osteoarthritis in the knee or elbow-topical NSAIDs work just as well as pills in most studies. One 2023 review found 18-92% of users reported good pain relief, depending on the product and how it was used. The key? Proper application. You need about a 4-6 inch ribbon of gel, applied 3-4 times a day. Too little? No effect. Too much? Risk of side effects.
Oral meds give more consistent results because they’re absorbed the same way every time. But topical? It depends on your skin type, temperature, and even the weather. One Reddit user in the r/ChronicPain community wrote, “My gel works fine in summer, but in winter? It barely feels like it’s doing anything.” That’s real. Skin absorbs drugs better when it’s warm. Cold weather slows absorption.
And let’s not forget: topical meds can’t reach deep joints or internal organs. If your pain comes from inside your hip or your spine, a cream won’t cut it. Oral meds still win for widespread or systemic conditions.
Who Benefits Most From Topical Medications?
Not everyone. But for some groups, topical meds are a game-changer.
Older adults? The American Geriatrics Society’s 2023 Beers Criteria says topicals should be first-line for seniors. Why? Because they cut the risk of GI bleeding by 82% compared to pills. For someone on blood thinners or with a history of ulcers, that’s life-saving.
People with swallowing issues? Topical forms have 37% higher adherence rates, according to a 2023 study of Medicare patients. No pills to choke down. No worrying about timing with meals.
Those who’ve had bad reactions to oral NSAIDs? Switching to topical often means relief without the side effects. In the same Arthritis Foundation survey, 78% of people who quit oral NSAIDs did so because of stomach problems. Only 22% stopped topicals-and most of them said it was because the pain was too severe for the cream to handle.
But here’s what’s often overlooked: topical meds aren’t just for pain. Antibiotic creams for infected cuts, steroid creams for eczema, and even hormone patches for menopause-all rely on controlled, localized delivery. They’re not alternatives to pills. They’re better tools for specific jobs.
What You’re Not Being Told About Application
Most people don’t use topical meds correctly. And that’s why they fail.
A 2023 survey of pharmacists found 41% of topical treatment failures were due to under-dosing or wrong frequency. People think a pea-sized amount is enough. It’s not. You need a ribbon the length of your index finger. Apply it only to the painful area. Wash your hands after. Don’t cover it with a bandage unless instructed.
Also, timing matters. Some gels work best on clean, dry skin. Others need to be rubbed in for 30 seconds to activate. And don’t apply right after a shower-wet skin dilutes the drug. Wait until your skin is cool and dry.
And here’s a hidden issue: OTC topical products often give vague instructions. The FDA found only 43% of over-the-counter creams include clear guidance on how much to use or how long to wait before washing. Oral meds? 89% have precise dosing. That’s a huge gap in patient education.

The Future: What’s Coming Next
The market is shifting fast. In 2023, the global topical drug market hit $52.3 billion-growing at 7.2% a year. Oral meds? Only 4.8%. Why? Because safety is now the top priority.
New tech is making topical delivery smarter. The FDA just approved Diclonate P, a diclofenac gel with 3.2 times better skin penetration than older versions. Still, it keeps blood levels under 5% of what an oral pill would do. That’s the sweet spot: effective locally, safe systemically.
And then there’s microneedle patches-tiny needles you wear like a bandage that dissolve under the skin, delivering drugs directly into the bloodstream without pills. Early trials show promise for osteoporosis meds, diabetes drugs, and even vaccines. These could bridge the gap between topical and oral delivery.
But there’s a limit. Drugs heavier than 500 Daltons can’t easily pass through skin. That’s why most antibiotics, antidepressants, and heart meds still come as pills. Science is working on it, but the skin is a tough barrier.
Choosing the Right Option for You
So which should you pick?
- Choose topical if: your pain is in one spot (knee, elbow, wrist), you’re over 65, you have stomach issues, or you’re taking other meds that increase bleeding risk.
- Choose oral if: your pain is widespread, you have deep joint or internal inflammation, or topical meds haven’t worked after 2 weeks of correct use.
Don’t assume one is better than the other. They’re different tools. Topical meds reduce hospitalizations. Oral meds treat what topicals can’t reach. The best choice isn’t about which is stronger-it’s about which fits your body and your life.
And if you’re unsure? Talk to your pharmacist. They see what works-and what doesn’t-every day. No guesswork needed.
Are topical medications safer than oral ones?
Yes, for most people, topical medications are significantly safer when used correctly. They deliver medication directly to the affected area with minimal absorption into the bloodstream. This reduces the risk of serious side effects like stomach ulcers, bleeding, and kidney damage-common with oral NSAIDs. Studies show topical NSAIDs cause less than 1% gastrointestinal side effects, compared to 15% with oral versions.
Can topical meds cause side effects?
Yes, but they’re usually mild. The most common side effect is skin irritation, redness, or itching at the application site, affecting 10-15% of users. In rare cases, applying too much over large areas-especially on broken or thin skin-can lead to systemic absorption, causing dizziness, nausea, or even liver stress. Always follow dosing instructions and avoid covering the area with tight bandages unless directed.
Why doesn’t my topical cream work as well as my pill?
Topical creams are designed for localized pain, not full-body conditions. If your pain comes from deep joints, your spine, or multiple areas, a cream won’t reach the source. Also, incorrect application is a big reason for failure-using too little, not applying often enough, or applying to wet skin can reduce effectiveness. Most people need a 4-6 inch ribbon applied 3-4 times daily for results.
Can I use topical and oral meds together?
Sometimes, yes-but only under medical supervision. Combining them can increase the total drug load in your system, raising the risk of side effects. For example, using both a topical NSAID and an oral NSAID can double your exposure to the same chemical. Always check with your doctor or pharmacist before mixing delivery methods, even if they seem harmless.
Are topical medications covered by insurance?
Yes, most insurance plans, including Medicare Part D, cover topical NSAIDs. In fact, 82% of 2023 Medicare formularies included topical NSAIDs, compared to 67% for oral versions. Out-of-pocket costs are often similar-around $12 for topical vs. $10 for generic oral pills. Some plans even prefer topicals due to lower long-term health risks, so ask your pharmacist about prior authorization options.
How long does it take for topical meds to work?
Most topical NSAIDs start working within 30 minutes to 2 hours, but full relief can take 3-7 days of consistent use. Unlike oral pills, which hit peak levels quickly, topicals build up slowly in the tissue. Don’t expect instant results. If you don’t feel improvement after 1-2 weeks of correct use, talk to your provider-it might not be the right treatment for your condition.
Do topical medications work better in warm weather?
Yes. Skin absorbs topical medications more efficiently when it’s warm. Studies show absorption increases significantly above 32°C (89.6°F). That’s why some users report less effectiveness in winter or cold environments. To improve absorption, apply the product after warming the area with a warm towel or during the warmest part of the day. Avoid applying right after a cold shower.

