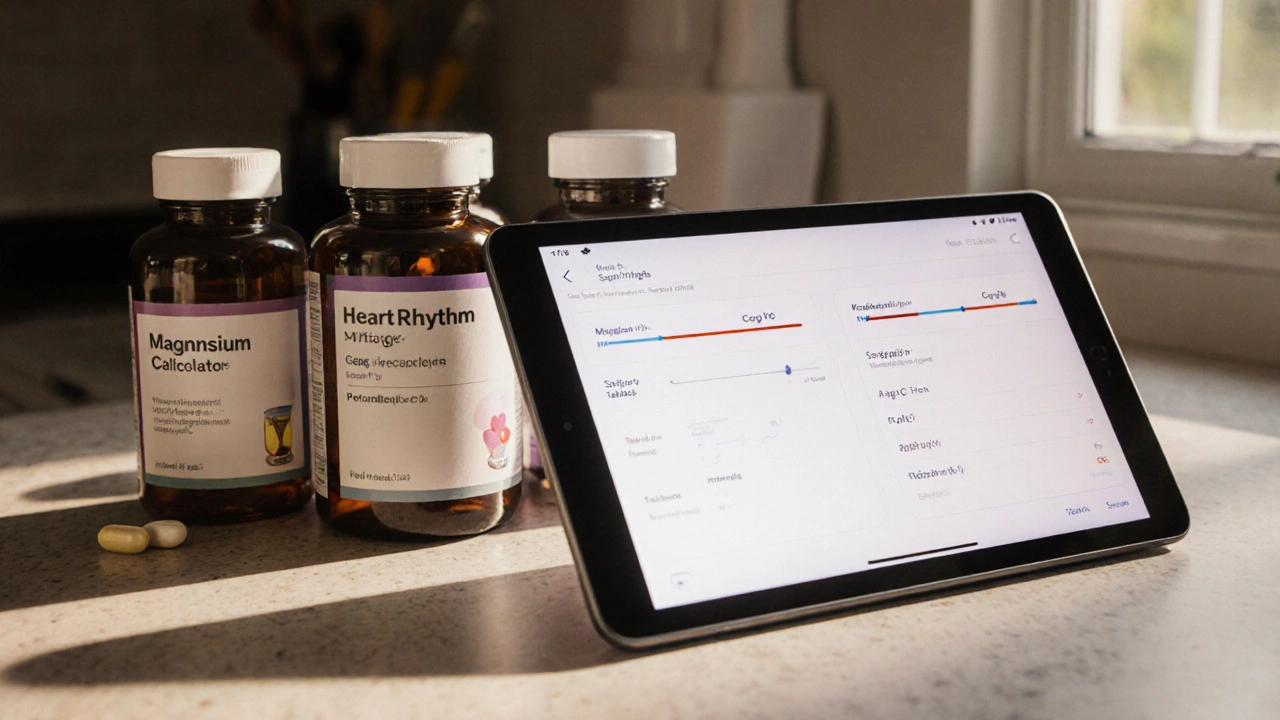
Heart Rhythm Supplement Calculator
Recommended Supplement Doses
Omega-3 (EPA/DHA): 1000 mg
Magnesium: 300 mg
CoQ10 (Ubiquinol): 100 mg
Potassium: 99 mg
Omega-3
Reduces inflammation and stabilizes cell membranes
Magnesium
Promotes electrical relaxation
CoQ10
Antioxidant protection for heart cells
Potassium
Maintains electrical gradient
Key Takeaways
- Supplements like omega‑3, magnesium, CoQ10, and potassium can improve heart rhythm stability.
- Evidence varies: omega‑3 has the strongest clinical backing, while magnesium helps with muscle relaxation.
- Choose high‑quality, third‑party tested products and watch for interactions with prescription meds.
- Supplements work best alongside a heart‑friendly diet, regular exercise, and stress management.
- Consult a healthcare professional before starting any new supplement regimen.
Living with an irregular heartbeat (a condition where the heart beats too fast, too slow, or unevenly) can feel unpredictable. While medication and lifestyle changes are the mainstays, many people wonder if a pill bottle on the kitchen counter can make a difference. The answer isn’t a simple yes or no-it depends on the type of supplement, the underlying cause of the arrhythmia, and how the supplement is used.
Understanding Irregular Heartbeat (Arrhythmia)
An arrhythmia occurs when the electrical signals that steer the heart’s pumping action become disorganized. Common triggers include electrolyte imbalances, high blood pressure, stress, caffeine, and certain medications. Symptoms range from occasional palpitations to fainting spells, and in severe cases, the heart may struggle to supply enough blood to the body.
Doctors often categorize arrhythmias by speed (tachycardia vs. bradycardia) or origin (atrial vs. ventricular). Knowing the specific type helps determine whether a supplement might help calm the rhythm or if a prescription is required.
Why Supplements Can Support Heart Rhythm
Heart‑healthy supplements target the same factors that spark irregular beats: inflammation, oxidative stress, and electrolyte balance. By supplying nutrients that the body either uses up quickly or struggles to absorb, supplements can shore up the cardiovascular system’s electrical stability.
Below are the four supplements with the most research backing for arrhythmia support.
Omega‑3 Fatty Acids
Omega‑3 fatty acids-primarily eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)-are found in fatty fish and fish‑oil capsules. They reduce inflammation, lower triglycerides, and improve cell‑membrane fluidity, which helps electrical signals travel smoothly.
Clinical trials (e.g., the GISSI‑Prevenzione study) showed a 15‑20% drop in sudden cardiac death among patients taking 1g of EPA/DHA daily. A 2023 meta‑analysis of 12 randomized controlled trials confirmed a modest but significant reduction in ventricular ectopy for people with mild arrhythmias.
Typical dose: 1,000-2,000mg of combined EPA/DHA per day, taken with meals to enhance absorption.
Side effects are rare but can include mild fishy aftertaste or gastrointestinal upset. High doses may thin the blood, so anyone on anticoagulants should check with a clinician.
Magnesium
Magnesium is a mineral that acts as a natural calcium blocker, helping the heart muscle relax between beats. Deficiencies are common, especially among people on diuretics or those who consume a lot of processed foods.
Research published in the Journal of the American College of Cardiology (2022) found that magnesium supplementation (400mg of elemental magnesium per day) cut the frequency of premature ventricular contractions by almost 30% in athletes with exercise‑induced arrhythmias.
Best forms for absorption are magnesium glycinate and magnesium citrate. Avoid magnesium oxide unless you need a laxative effect, as it’s poorly absorbed.
Excess magnesium can cause diarrhea and, in extreme cases, heart block, so stay within the Recommended Dietary Allowance (RDA) unless advised otherwise.
Coenzyme Q10 (CoQ10)
Coenzyme Q10 is a co‑factor in cellular energy production and a powerful antioxidant. It helps protect heart cells from oxidative damage that can disrupt electrical pathways.
In a double‑blind trial with 120 patients suffering from atrial fibrillation, 200mg of ubiquinol (the reduced, more absorbable form of CoQ10) taken nightly reduced the number of symptomatic episodes by 22% over six months.
CoQ10 is especially useful for people on statins, which can lower natural CoQ10 levels and sometimes worsen muscle cramps or fatigue.
Typical dosage: 100-200mg per day, split into two doses if stomach sensitivity occurs.
Potassium
Potassium is essential for maintaining the heart’s electrical gradient. Low potassium (hypokalemia) is a known trigger for both atrial and ventricular arrhythmias.
Guidelines from the American Heart Association (2024) recommend 4,700mg of potassium daily for adults, primarily from food sources like bananas, sweet potatoes, and leafy greens. When diet falls short, a low‑dose supplement (e.g., 99mg of potassium chloride) can safely fill the gap.
High‑dose potassium supplements (>200mg) should only be used under medical supervision because of the risk of hyperkalemia, which can cause dangerous arrhythmias.
Choosing the Right Supplement
Not every supplement suits every person. Use these criteria to decide:
- Evidence level: Prioritize ingredients with randomized controlled trials (Omega‑3, magnesium).
- Formulation quality: Look for third‑party testing (USP, NSF) to verify potency.
- Interaction potential: Check if you’re on blood thinners, beta‑blockers, or diuretics.
- Personal health profile: Age, kidney function, and existing heart conditions influence safe dosages.
Potential Risks and Interactions
While many people tolerate these nutrients well, there are a few red flags:
- Blood thinners: Omega‑3 and high‑dose magnesium can increase bleeding risk.
- Kidney disease: Potassium and magnesium accumulation may become harmful.
- Medication timing: Some supplements (e.g., magnesium) can interfere with the absorption of certain antibiotics or thyroid meds.
Always discuss new supplements with a cardiologist or primary‑care provider, especially if you’re already on prescription anti‑arrhythmic drugs.
Putting Supplements into a Heart‑Friendly Lifestyle
Supplements work best when they complement a solid foundation:
- Nutrition: Emphasize whole foods rich in omega‑3 (salmon, walnuts), potassium (avocados, beans), and magnesium (nuts, seeds).
- Exercise: Regular aerobic activity (30minutes most days) improves heart rhythm stability.
- Stress management: Techniques like deep breathing, yoga, or mindfulness lower catecholamine spikes that trigger palpitations.
- Sleep hygiene: Aim for 7-9hours; sleep deprivation can increase arrhythmia risk.
Comparison of Top Heart‑Healthy Supplements
| Supplement | Primary Heart Benefit | Typical Daily Dose | Evidence Strength | Common Side Effects |
|---|---|---|---|---|
| Omega‑3 (EPA/DHA) | Reduces inflammation, stabilizes cell membranes | 1,000-2,000mg | High (multiple RCTs) | Fishy aftertaste, mild GI upset |
| Magnesium (glycinate) | Promotes electrical relaxation, prevents ectopy | 300-400mg elemental Mg | Moderate (observational & RCT data) | Diarrhea, occasional cramping |
| CoQ10 (ubiquinol) | Antioxidant protection of cardiac cells | 100-200mg | Moderate (small RCTs) | Insomnia, mild stomach upset |
| Potassium (low‑dose) | Maintains proper electrical gradient | 99mg (supplement) + food sources | Low (mostly dietary guidelines) | Hyperkalemia if overdosed |
Troubleshooting Common Issues
Feeling no effect after a month? Most studies show benefits after 8-12weeks. Check that you’re taking a high‑quality product, and confirm the dose matches the research.
Digestive upset? Try switching to a different form (e.g., magnesium glycinate instead of citrate) or take the supplement with food.
Worried about interactions? Keep a simple log of all meds and supplements, then review it with your doctor. Apps like Medisafe can flag known conflicts.
Frequently Asked Questions
Can supplements replace prescription meds for irregular heartbeat?
No. Supplements are adjuncts that may improve rhythm stability, but they don’t treat the underlying electrical disorder the way anti‑arrhythmic drugs do. Always follow a doctor’s prescription.
How long before I notice a change?
Most studies report measurable improvements after 8 to 12 weeks of consistent use. Patience and adherence are key.
Are there any heart‑healthy supplements I should avoid?
Avoid high‑dose potassium or magnesium if you have kidney disease, and steer clear of fish‑oil products that aren’t molecularly distilled if you’re on blood thinners. Always verify purity.
Should I take these supplements together?
Yes, many people stack omega‑3, magnesium, and CoQ10 without issues. Separate potassium doses from other minerals to improve absorption-take potassium at a different time of day.
What’s the best time of day to take them?
Omega‑3 and CoQ10 are best with meals to aid absorption. Magnesium can be taken in the evening to support sleep. Potassium works well with food, so a midday snack is ideal.
Bottom line: heart‑healthy supplements can be a practical, evidence‑backed tool for people living with an irregular heartbeat, but they work best when paired with a balanced diet, regular activity, and professional medical guidance.