Stress and Anal Itch Severity Calculator
Your Analysis Results
Ever notice that a harmless-looking bite on the lower back end suddenly feels like a thousand tiny needles when you’re stressed? That’s not just coincidence. Your body’s response to stress can turn a mild irritation into a relentless itch that makes sitting uncomfortable and sleep elusive. Below we’ll unpack why stress amplifies anal itching after an insect bite, how to spot the warning signs, and practical steps you can take to calm both mind and skin.
What actually happens when an insect bites the anal area?
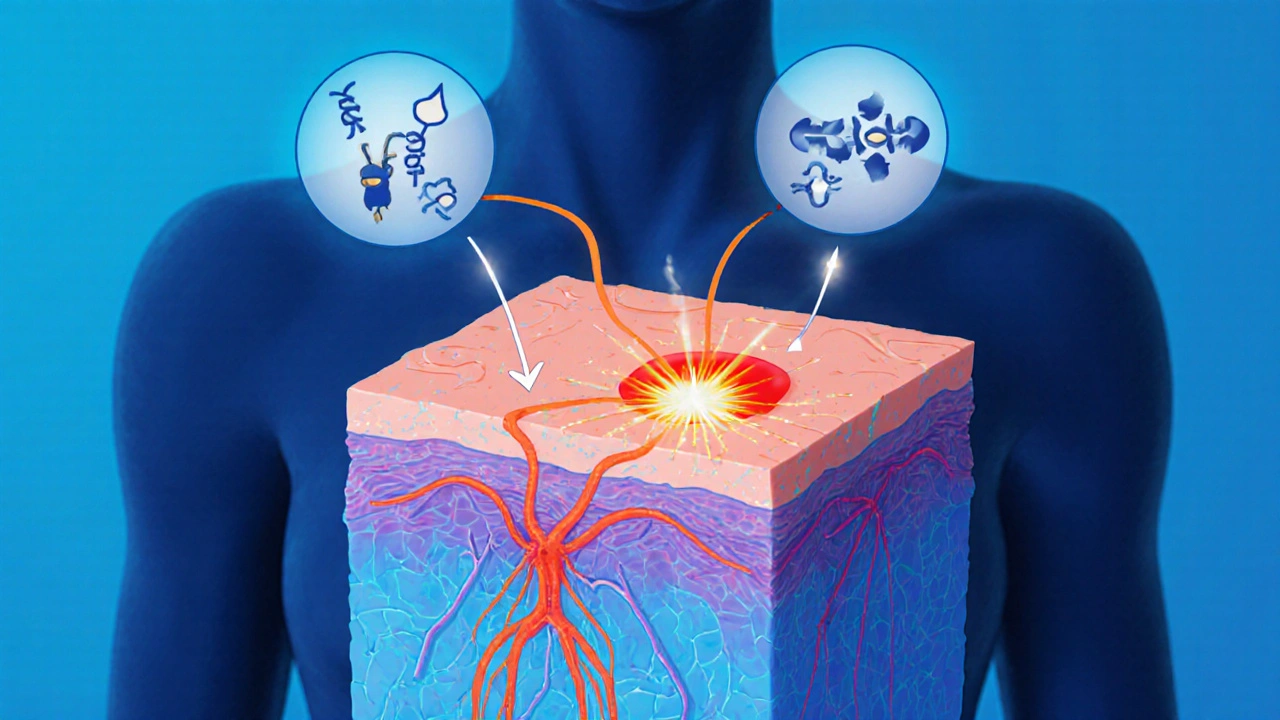
When a mosquito, flea, or bite‑producing insect lands on the delicate skin around the anus, it injects saliva that contains anticoagulants and proteins designed to keep blood flowing. Your immune system reacts by releasing histamine (a chemical that dilates blood vessels and creates the classic redness and swelling). Histamine also activates nerve endings that signal the brain: “Hey, something’s wrong-scratch it!” In the anal region, the skin is thinner and more sensitive, so the itch can feel especially intense.
How does stress turn a mild itch into a burning nuisance?
Stress isn’t just a feeling; it’s a cascade of hormones and neural signals. When you’re under pressure, the hypothalamic‑pituitary‑adrenal (HPA) axis releases cortisol (the body’s primary stress hormone). While cortisol can calm inflammation in the short term, chronic elevation does the opposite: it weakens the skin barrier, disrupts the gut‑skin axis, and boosts production of pro‑inflammatory cytokines like interleukin‑6 (IL‑6). These cytokines sensitize the nociceptors (pain‑and‑itch detecting nerves) in the anal tissue, making the itch feel louder.
At the same time, stress triggers the sympathetic nervous system-think “fight‑or‑flight.” Blood flow is shunted away from the lower gut and perianal skin, slowing healing and allowing the bite’s irritants to linger. The result? A feedback loop where stress intensifies itching, itching raises anxiety, and the cycle spirals.
Key signs that stress is amplifying your anal itch
- Itch worsens during high‑stress moments (work deadlines, arguments, or sleepless nights).
- Scratching leads to visible redness, swelling, or even tiny cracks in the skin.
- Other stress‑related symptoms appear-headaches, muscle tension, or digestive upset.
- The itch feels “burning” rather than the typical “tickle” of a simple bite.
If you notice these patterns, you’re likely dealing with a psychosomatic response (a physical symptom driven or worsened by mental stress). Recognizing the link is the first step toward breaking it.
Immediate relief: What to apply and when
For fast itch suppression, start with over‑the‑counter options:
- Apply a hydrocortisone cream (a mild topical steroid that reduces inflammation) 1% to the affected area, no more than three times a day.
- Use an calamine lotion (soothes skin and dries out weeping lesions) after the steroid has dried.
- Take an oral antihistamine like loratadine (10mg) if the itch is widespread.
These measures tackle the histamine surge but won’t address the stress component. That’s why pairing them with stress‑management techniques produces the most lasting relief.
Stress‑management tools that calm the itch
| Method | Time Needed | Evidence Strength | Typical Benefit for Itch |
|---|---|---|---|
| Deep‑breathing (4‑7‑8 technique) | 5minutes | Moderate | Quick reduction in cortisol spikes |
| Progressive muscle relaxation | 10‑15minutes | Strong | Decreases overall muscle tension, easing scratching urge |
| Mindful meditation | 10‑20minutes daily | Strong | Lowers IL‑6 levels, softens nerve sensitivity |
| Cognitive‑behavioral therapy (CBT) worksheets | 30minutes weekly | Strong | Helps reframe itch‑related anxiety, breaking the feedback loop |
| Gentle walking or light cardio | 20‑30minutes | Moderate | Improves circulation to the perianal area, promoting healing |
Pick one that fits your routine and stick with it for at least a week. You’ll often notice the itch receding as your stress hormones settle.
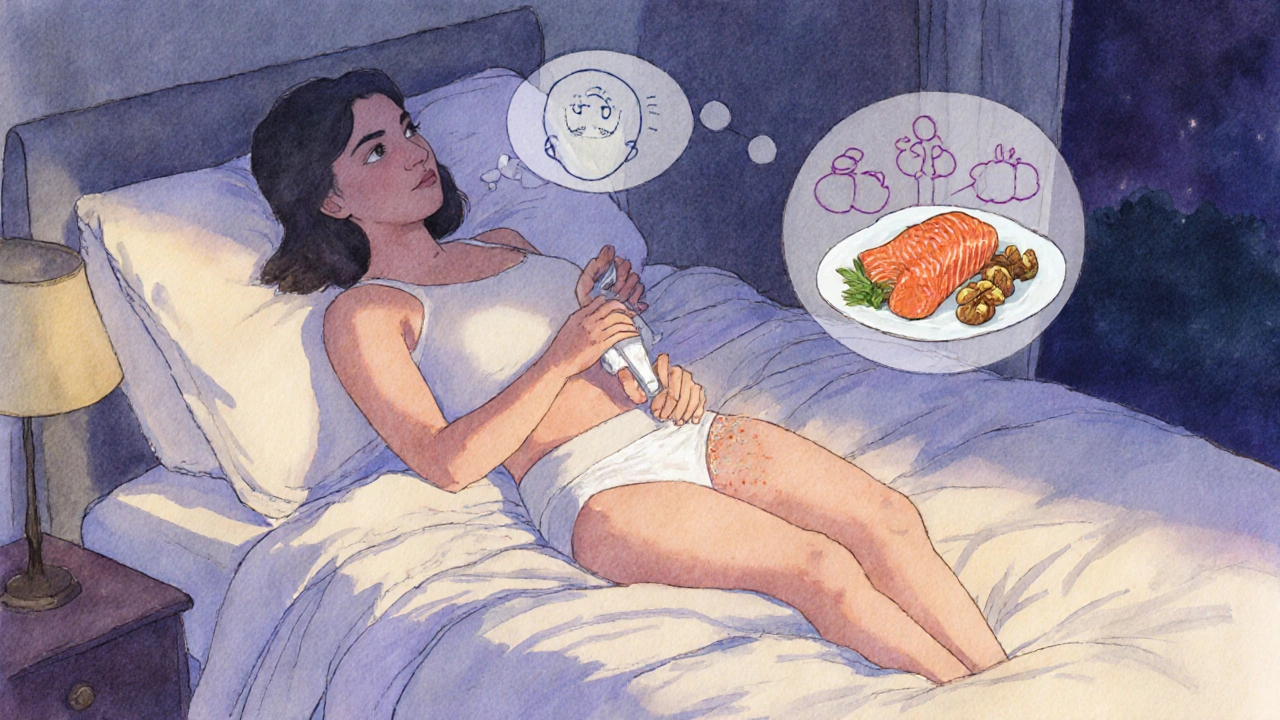
Diet and gut health: The hidden players
The gut‑skin axis is a hot research area. A diet high in processed sugars can fuel systemic inflammation, raising IL‑6 and worsening itch. Conversely, foods rich in omega‑3 fatty acids (salmon, walnuts) and antioxidants (berries, leafy greens) support a balanced immune response. Probiotic‑rich foods like kefir or a daily 5‑billion‑CFU supplement can help maintain a healthy microbiome, which in turn stabilizes the HPA axis.
When to see a healthcare professional
If any of the following occur, schedule an appointment:
- Itch persists longer than two weeks despite topical treatment.
- Signs of infection appear-pus, severe swelling, fever.
- Bleeding or severe skin breakdown from scratching.
- Stress symptoms interfere with daily functioning (sleep loss, constant anxiety).
A clinician might prescribe a stronger topical steroid, a short course of oral steroids, or refer you to a dermatologist for patch testing to rule out allergic contact dermatitis.
Preventing future bites in the anal region
While you can’t control every insect, you can reduce exposure:
- Wear breathable cotton underwear; tight synthetic fabrics retain moisture, which attracts flies and mosquitoes.
- Apply an EPA‑registered insect repellent containing 20‑30% DEET or picaridin to the groin area before outdoor activities.
- Keep your bathroom and bedroom screens in good repair; seal cracks around windows.
- Use a fan or air conditioner at night; many biting insects avoid cool breezes.
These steps, combined with regular stress‑reduction practice, give you the best defense against a repeat episode.
Frequently Asked Questions
Can anxiety alone cause anal itching without a bite?
Yes. Anxiety can heighten nerve sensitivity and trigger a psychosomatic itch, especially in areas with dense nerve endings. However, most cases have an underlying irritant, so a quick skin check is wise.
Is it safe to use hydrocortisone cream near the anus?
A 1% hydrocortisone cream applied sparingly is generally safe for short‑term use (up to 7 days). Avoid using it on broken skin for longer periods without medical supervision.
Do antihistamines help with stress‑related itch?
Antihistamines block the histamine pathway, so they reduce the immediate allergic component. They don’t lower cortisol, but the calmer you feel, the less you’ll scratch, breaking the cycle.
How long should I practice stress‑management techniques before seeing improvement?
Most people notice a drop in itch intensity after 5‑7 days of consistent practice. If the itch remains severe after two weeks, evaluate other factors like infection or allergic reactions.
Are there natural remedies that work better than OTC creams?
Aloe vera gel applied cool can soothe inflammation, and oatmeal baths (colloidal oatmeal) reduce itching. These are gentle adjuncts, but they don’t replace a steroid if the inflammation is strong.

