When a pharmacist swaps a brand-name pill for a generic version, it’s not just a cost-saving move-it’s a clinical decision. For kids and older adults, that switch can mean the difference between taking medicine as prescribed and stopping it altogether. The problem isn’t that generics are less effective. They’re not. But how you explain the change matters more than you think.
Why Generic Substitution Isn’t as Simple as It Looks
Generic drugs have the same active ingredient, strength, and route of delivery as their brand-name counterparts. The FDA requires them to be within 80-125% of the brand’s absorption rate. That sounds precise. But for a 3-month-old with reflux or an 82-year-old on five different drugs, even a 20% variation can cause real problems. Take lansoprazole (Prevacid) for GERD. The brand comes in a pediatric-friendly sprinkle capsule. The generic? Often a capsule that’s harder to open, or a tablet that’s too big for a toddler to swallow. A 2019 FDA report found only 32% of generic pediatric formulations are available as liquids or chewables-compared to 68% of brand-name versions. That’s not a technical gap. It’s a compliance gap. For seniors, it’s worse. One man in Oregon told his pharmacist he stopped taking his blood pressure pill because it changed color three times in six months. He thought he was getting a different drug. He wasn’t. But he didn’t know that. He’d been on the same brand for 12 years. Suddenly, the shape, size, and color shifted. No one warned him. He stopped. His blood pressure spiked. He ended up in the ER.What Parents Really Worry About (And What Doctors Don’t Tell Them)
A 2020 study in Pediatrics found 62% of parents hesitate to accept generic meds for their kids. Why? Taste. Texture. Fear. One mother on Reddit shared her story: her 2-year-old refused the generic amoxicillin because it tasted like “burnt metal.” The brand version was sweetened and flavored. The generic? Bitter. He gagged. She gave up. She switched back-despite the $40 difference per prescription. Doctors often say, “It’s the same medicine.” But that’s not enough. Parents aren’t worried about bioequivalence. They’re worried about their child throwing up, refusing meds, or getting sicker. You need to say: “I know this looks different. The active ingredient is the same, but the flavor and texture changed. That’s why some kids don’t like it. We can try a different generic, or we can ask for a liquid version.” Don’t assume they know what “bioequivalence” means. Don’t use the word “generic” like it’s a reassurance. Say: “This is a lower-cost version of the same medicine. It works the same way, but it might taste different.” Then pause. Let them ask.What Seniors Need-And Why They Don’t Tell You
Seniors take an average of 4.8 prescription drugs. Many have memory issues, vision loss, or hearing trouble. A 2021 study in Frontiers in Pharmacology found 58% of seniors report new side effects after switching to a generic-even when no pharmacological change occurred. That’s the nocebo effect: believing something will make you feel worse, so you do. A 78-year-old woman in Portland stopped her statin because the pill went from blue to white. She thought it was a counterfeit. She didn’t tell her doctor. She just stopped. Her cholesterol jumped. She didn’t connect the dots. Here’s what works: Proactive communication. Don’t wait until they notice the pill looks different. Call them before the refill. Say: “Your next bottle of simvastatin will have a different shape and color. That’s because we’re using a different manufacturer. The medicine is the same. It’s just packaged differently.” Use large-print labels. Include a small picture of the pill on the label. Offer a printed card with the name, color, shape, and imprint of each pill they take. If they live with family, involve a caregiver. A 2022 study showed 32% better adherence when family members were part of the conversation.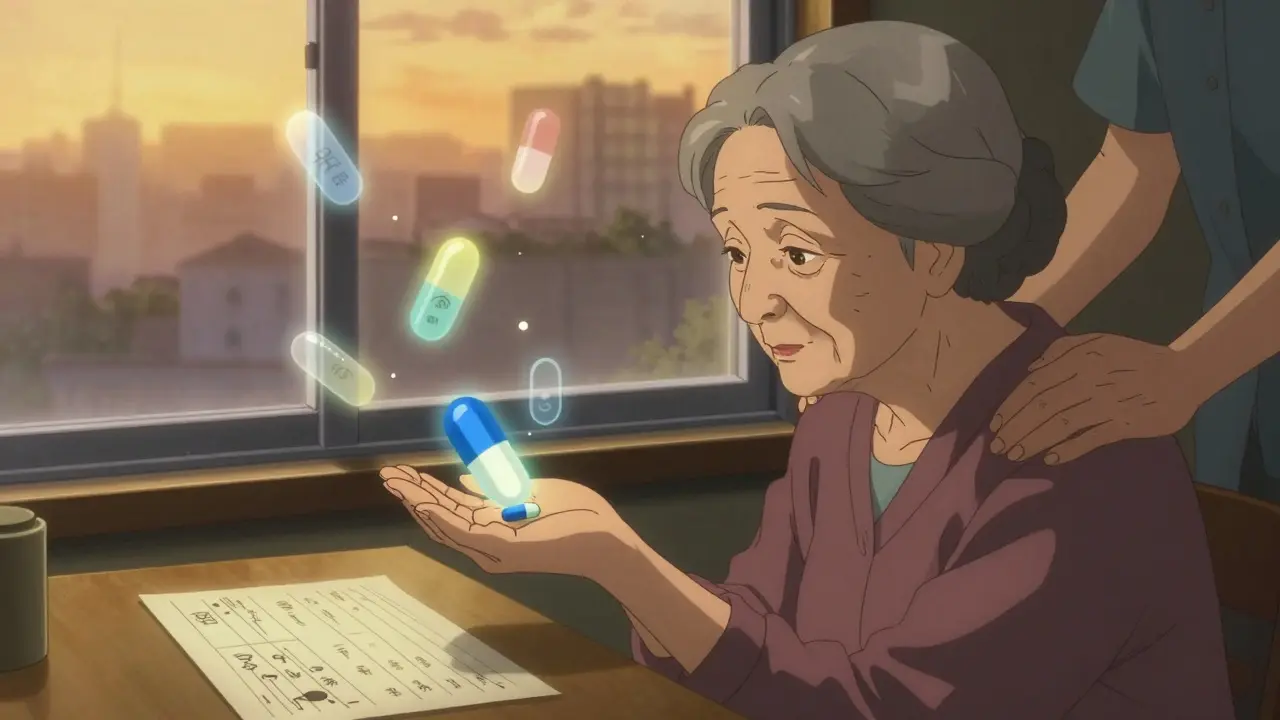
The Teach-Back Method: The Most Underused Tool in Medicine
The teach-back method isn’t fancy. It’s simple: ask the patient to explain it back to you. Instead of: “This is the same medicine.”Say: “I want to make sure I explained this right. Can you tell me in your own words why we’re switching to this pill?” If they say, “I don’t know,” or “It’s cheaper, right?”-you haven’t communicated. You’ve just handed over a pill. For kids: Ask the parent. “What would you tell your child about this new pill?” If they say, “I’d say it’s the same,” but they’re nervous-dig deeper. “What worries you most?” For seniors: Use plain language. No jargon. No “bioequivalence.” Say: “This pill has the same medicine inside. It just looks different because it’s made by another company. It works the same way.” Then ask them to repeat it. A 2021 NIH study found this method cut medication errors by 29%. That’s not a small win. That’s life-changing.
When Generic Substitution Should Be Avoided
Not every drug is safe to swap. For drugs with a narrow therapeutic index-like seizure meds (phenytoin, carbamazepine), blood thinners (warfarin), or thyroid meds (levothyroxine)-even tiny changes in absorption can cause seizures, clots, or thyroid crashes. A 2017 Danish study followed nine epilepsy patients who switched generics. Four had seizure relapses. The pills were technically “bioequivalent.” But their bodies reacted differently. One patient had a seizure while driving. He almost died. The FDA doesn’t ban these switches. But many states are starting to. As of 2024, 28 states are considering laws to block automatic substitution for these drugs in kids and seniors. If your patient is on one of these, don’t assume substitution is okay. Ask: “Has this patient had stable control for over a year?” If yes, leave it alone. If no, stick with the brand-or get a specialist involved.
What’s Changing in 2026
The FDA launched its Generic Drug Communications Initiative in 2023. New rules require manufacturers to include clear, plain-language info about formulation differences in patient handouts. That means pill color, shape, and taste changes must now be explained-not buried in fine print. Pharmacists are getting better training too. The American Society of Health-System Pharmacists updated its guidelines in January 2024. They now require:- Verbal counseling before substitution for seniors and children
- Use of visual aids (pill images, color charts)
- Documentation of patient understanding in the record
What You Can Do Today
You don’t need new tools. You need better habits.- For kids: Always ask about taste. Offer alternatives. If the generic tastes awful, call the prescriber. Maybe there’s a different generic with better flavor.
- For seniors: Use the teach-back method. Give them a pill card. Involve a family member. Don’t wait for them to notice the change-tell them before.
- For both: Never say “It’s the same.” Say “It has the same medicine inside, but it looks different because it’s made by another company.”
- For all: Document the conversation. Not just “patient counseled.” Write: “Explained pill change. Parent understood. No concerns.”
What Patients Want
A 2023 study in Frontiers in Pharmacology found 76% of patients believe they should have the right to choose between brand and generic-even if it costs more. That’s not just about money. It’s about control. About trust. You can’t always give them the brand. But you can give them honesty. You can give them time. You can give them a voice. That’s how you turn a cost-saving move into a healing one.Are generic drugs really as good as brand-name drugs for kids and seniors?
Yes-when the drug isn’t one with a narrow therapeutic index (like seizure or thyroid meds). The FDA requires generics to deliver the same active ingredient in the same amount, with absorption within 80-125% of the brand. But for children, the issue isn’t effectiveness-it’s formulation. Many generics lack kid-friendly forms like flavored liquids or chewables. For seniors, the problem is consistency. Switching between different-looking generics can cause confusion or stoppage, even if the medicine is identical.
Why do some children refuse generic medications?
Many generic liquid medications don’t have the same flavoring or texture as brand-name versions. A 2019 FDA review found only 32% of generic pediatric formulations are available as liquids or chewables, compared to 68% of brand-name ones. A bitter taste or gritty texture can make a child gag or refuse the medicine entirely, even if it’s medically identical. This leads to missed doses and worse outcomes.
Can switching to a generic cause side effects in older adults?
Not because of the drug itself-but because of perception. A 2021 study found 58% of seniors reported new side effects after switching to a generic, even when no pharmacological change occurred. This is called the nocebo effect: expecting something to make you feel worse makes you feel worse. Changing pill color, size, or shape without warning can trigger anxiety, confusion, or mistrust, leading patients to stop taking their medicine.
What’s the best way to explain a generic substitution to a senior?
Use simple language and the teach-back method. Say: “Your next pill will look different-it might be a different color or shape-but it has the same medicine inside. We’re switching because it’s less expensive, and it works the same way.” Then ask: “Can you tell me what you’ll do if you see a different pill next time?” Give them a printed card with the pill’s name, color, shape, and imprint. Involve a family member if possible.
Should I avoid generic drugs for my child with epilepsy?
Many experts recommend sticking with the same formulation-brand or generic-if your child’s seizures are well-controlled. Drugs like phenytoin and carbamazepine have a narrow therapeutic window, meaning even small changes in absorption can lead to seizures. A 2017 study showed some patients had seizure relapses after switching generics, even though the drugs met FDA standards. Talk to your neurologist before switching.
Is there a law that says pharmacists must tell me before switching to a generic?
It depends on your state. In 19 states, pharmacists must substitute generics automatically. In 7 states and Washington, DC, they need your consent. In 31 states, they must notify you after the switch. There’s no federal rule requiring advance notice. That’s why proactive communication from your doctor or pharmacist is so important-don’t wait for the law to protect you.

