SSRI and NSAID Interaction Risk Checker
This tool helps you understand the risk of gastrointestinal bleeding when taking both an SSRI antidepressant and an NSAID pain reliever together. Based on your medication choices and risk factors, we'll show you your risk level and provide personalized recommendations to stay safe.
Every year, millions of Americans take SSRIs for depression or anxiety and NSAIDs for back pain, arthritis, or headaches. It seems harmless-two common meds, one for mood, one for pain. But when taken together, they can silently raise your risk of a life-threatening bleed in your stomach or intestines. This isn’t rare. It’s common. And most people don’t know about it.
Why This Combination Is Dangerously Common
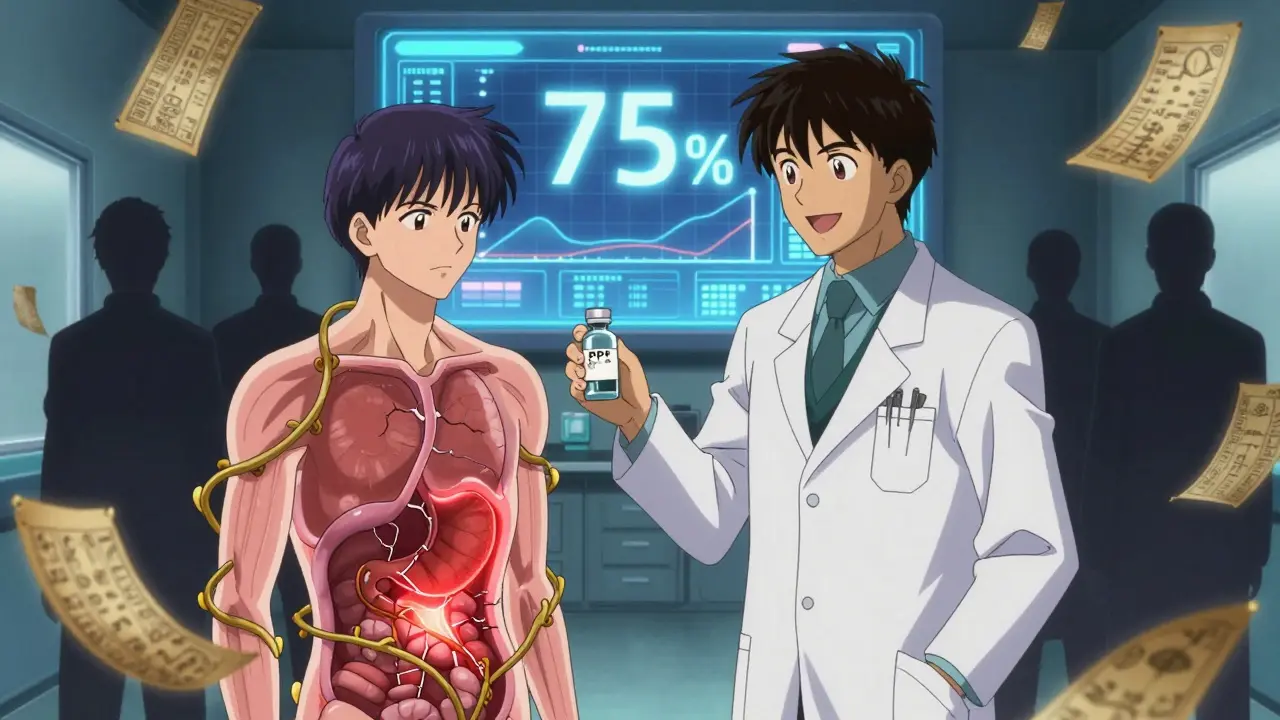
SSRIs like sertraline, fluoxetine, and escitalopram are among the most prescribed antidepressants in the U.S. About 34.7 million adults took them in 2021. NSAIDs like ibuprofen, naproxen, and diclofenac are even more widespread-17 million Americans use them daily for chronic pain. The overlap is huge. A 2022 audit of over 2 million patient records found that nearly 28% of people on SSRIs were also prescribed NSAIDs within six months. That’s almost 9.8 million people in the U.S. alone taking a combination that increases their risk of upper GI bleeding by 75%.This isn’t just a theoretical risk. People are ending up in the ER with black, tarry stools, vomiting blood, or sudden dizziness from internal bleeding. One Reddit user described three days of dark stools before seeking help. Another reported a hospital stay after taking sertraline and ibuprofen for a week. These aren’t outliers-they’re predictable outcomes of a poorly understood drug interaction.
How SSRIs and NSAIDs Work Together to Cause Bleeding
Each drug alone increases bleeding risk. Together, they multiply it.SSRIs block serotonin reuptake in platelets. Serotonin helps platelets clump together to stop bleeding. Without it, your blood takes longer to clot when a small vessel in your stomach lining gets irritated. It’s like having a slow-acting anticoagulant you didn’t know you were on.
NSAIDs attack the stomach’s natural defenses. They block COX-1, an enzyme that makes protective prostaglandins. These prostaglandins keep the stomach lining thick with mucus and blood flowing to repair damage. When they’re gone, your stomach lining becomes thin and vulnerable-even to normal stomach acid.
Put them together: your stomach lining is damaged by NSAIDs, and your blood can’t clot properly because of SSRIs. The result? A bleed that starts small, goes unnoticed, and can quickly become severe. Studies show this combo raises bleeding risk more than either drug alone-sometimes as much as 12 times in high-risk groups. That’s not just a side effect. It’s a dangerous synergy.
Not All SSRIs or NSAIDs Are Equal
The risk isn’t the same across every medication in these classes.Among NSAIDs, ibuprofen carries the lowest GI bleeding risk among non-selective options. Naproxen and diclofenac are significantly worse. Ketorolac and piroxicam are the riskiest. Celecoxib, a COX-2 inhibitor, is much safer-its bleeding risk is close to baseline, with an odds ratio of just 1.16 compared to 2.5-4 for traditional NSAIDs.
For SSRIs, most carry similar risks because they all affect platelet serotonin. But some data suggests escitalopram and citalopram may have slightly lower bleeding potential than fluvoxamine or paroxetine. It’s not enough to switch blindly, but if you’re already on an SSRI and need pain relief, knowing this helps guide smarter choices.
The real danger isn’t the drugs themselves-it’s the combination. Monotherapy with an SSRI increases bleeding risk by about 40-50%. Monotherapy with a high-risk NSAID can double or triple it. Together? It’s not 40% + 200%. It’s 75% higher than what you’d expect from either alone. That’s multiplicative, not additive.
Who’s Most at Risk?
Not everyone taking both drugs will bleed. But certain people are in the danger zone:- People over 65
- Those with a history of ulcers or GI bleeding
- Patients on blood thinners like warfarin or aspirin (even low-dose)
- People with H. pylori infection
- Those taking high doses of NSAIDs or multiple NSAIDs
If you’re 70 and take sertraline for depression and naproxen for knee pain, your risk isn’t just elevated-it’s critical. The same combo might be low-risk for a healthy 35-year-old with occasional headaches. Age and prior history matter more than the drugs themselves.
What Doctors Should Be Doing (But Often Aren’t)
A 2021 survey of 1,200 primary care doctors found that only 38.7% routinely screen for SSRI-NSAID interactions. Just 22.3% prescribe protective meds like proton pump inhibitors (PPIs) when both are needed.Patients aren’t being warned. A 2022 Medscape survey of 452 patients showed 68% were never told about bleeding risks when prescribed both drugs. That’s not negligence-it’s systemic failure. This interaction has been known since at least 2002. The FDA added warnings to SSRI labels in 2019. The American College of Gastroenterology has clear guidelines. Yet most patients are left in the dark.
Doctors often assume the patient knows, or that the risk is too small to mention. But when 9.8 million people are on this combo, “small risk” becomes a public health crisis. The cost? $1.27 billion annually in U.S. hospital bills alone. Each bleed averages $15,642 in costs.

How to Prevent This Bleeding Risk
There are three proven ways to protect yourself if you need both drugs:- Switch your pain reliever. Try acetaminophen (Tylenol) instead of NSAIDs. It doesn’t affect platelets or the stomach lining. For arthritis or chronic pain, it’s often enough. If you need stronger relief, ask about topical NSAIDs (gels or patches)-they have far less systemic impact.
- Switch your NSAID. If you must use an NSAID, choose celecoxib. It’s the safest option. If celecoxib isn’t right for you, ibuprofen is the next best. Avoid naproxen, diclofenac, and ketorolac.
- Add a PPI. If you’re on both an SSRI and an NSAID, you should be on a proton pump inhibitor like omeprazole (20 mg daily) or pantoprazole. A 2023 meta-analysis showed PPIs cut the excess bleeding risk by 70%. That’s not a bonus-it’s essential.
Some patients report no issues after switching from naproxen to celecoxib and adding omeprazole while staying on sertraline. That’s not luck-it’s smart management.
What You Can Do Right Now
You don’t need to wait for your doctor to bring it up. Take action:- Check your medication list. Are you on both an SSRI and an NSAID?
- Look up your specific drugs. Is your NSAID ibuprofen or naproxen? Is your SSRI fluoxetine or escitalopram?
- Ask your pharmacist: “Am I at risk for stomach bleeding with these two?”
- Ask your doctor: “Should I be on a PPI with these medications?”
- If you’ve had black stools, vomiting blood, or unexplained fatigue, get checked now. Don’t wait.
Many people think GI bleeding only happens to heavy drinkers or older adults with ulcers. It doesn’t. It happens to someone who took ibuprofen for a sore back while on sertraline for anxiety. It happens quietly. And it can kill.
The Future: Better Tools and Safer Options
Progress is being made. Mayo Clinic and Cleveland Clinic now have automated alerts in their electronic records that flag SSRI-NSAID combos. Cleveland Clinic saw a 42% drop in GI bleeds after launching their alert system in 2020.New drugs are coming. TissueTech is testing a pill that combines ibuprofen with omeprazole in one capsule-designed to protect the stomach as you take the painkiller. AI models are being trained to predict individual bleeding risk with 86% accuracy using health records.
And soon, testing for H. pylori-a bacteria that causes ulcers-may become standard before starting dual therapy. If you have it, treating it can cut your bleeding risk in half.
But until these tools are everywhere, the responsibility falls on you. Don’t assume your doctor knows. Don’t assume it’s safe. Ask. Push back. Protect yourself.
This isn’t about avoiding medication. It’s about using it wisely. You need your antidepressant. You need pain relief. But you don’t need to risk bleeding to get it. There are safer paths. You just have to ask for them.
Can I take ibuprofen with sertraline?
You can, but it’s not safe without protection. Taking ibuprofen with sertraline increases your risk of upper GI bleeding by about 75%. If you must take both, you should also take a proton pump inhibitor like omeprazole daily. Consider switching to acetaminophen instead, or ask your doctor about celecoxib, which has a much lower bleeding risk.
What’s the safest NSAID to take with an SSRI?
Celecoxib is the safest NSAID to use with an SSRI. It’s a COX-2 inhibitor and has a bleeding risk close to baseline (odds ratio 1.16). Among traditional NSAIDs, ibuprofen carries the lowest risk, followed by naproxen and diclofenac, which are significantly more dangerous. Avoid ketorolac and piroxicam entirely if you’re on an SSRI.
Do all SSRIs increase bleeding risk the same way?
Most SSRIs affect platelet serotonin similarly, so their bleeding risk is generally comparable. However, some studies suggest escitalopram and citalopram may have slightly lower risk than fluvoxamine or paroxetine. This difference is small and not enough to rely on for safety. The bigger factor is whether you’re also taking an NSAID. If you are, the SSRI type matters less than adding a PPI.
How do I know if I’m having a GI bleed?
Signs include black, tarry stools (melena), vomiting blood or material that looks like coffee grounds, sudden dizziness, rapid heartbeat, or unexplained fatigue. These symptoms can be subtle at first. If you’re on both an SSRI and NSAID and notice any of these, seek medical help immediately. Don’t wait for severe pain-it’s often not present.
Should I stop my SSRI if I need NSAIDs?
No, don’t stop your SSRI without talking to your doctor. Stopping abruptly can cause withdrawal symptoms or a relapse of depression or anxiety. Instead, ask about safer alternatives: switch your NSAID to celecoxib or acetaminophen, or add a proton pump inhibitor. Your mental health matters-and it can be protected while reducing your bleeding risk.
Are there alternatives to SSRIs that don’t increase bleeding risk?
Yes. Bupropion (Wellbutrin) is an antidepressant that doesn’t affect platelet serotonin and doesn’t increase GI bleeding risk. If you’re on an SSRI and need NSAIDs long-term, talk to your doctor about switching to bupropion. It’s not right for everyone, but it’s a viable option for many, especially if you don’t have significant anxiety symptoms.

