Managing medications at home can be overwhelming-especially for seniors taking five, ten, or even more pills a day. Missed doses, wrong times, duplicate prescriptions, dangerous interactions-these aren’t just inconveniences. They lead to hospital visits, falls, confusion, and worse. The good news? Home health services for medication management are designed exactly for this problem. They’re not just about handing out pills. They’re about safety, consistency, and peace of mind.
What Home Health Medication Management Actually Does
Home health nurses and aides don’t just show up to hand you a cup of water and a pill. They follow a strict, evidence-based system. First, they create a complete, up-to-date list of every medication you’re taking-brand names, generics, dosages, why you’re taking it, and when. This isn’t just a piece of paper. It’s a living document shared with your doctor, pharmacist, and family. If your cardiologist adds a new blood thinner and your primary care doctor prescribes a painkiller, someone catches the interaction before it hurts you. According to MedPro’s 2022 analysis, professional medication management cuts adverse drug events by 60% compared to self-management. That’s not a guess. That’s data from thousands of cases. For seniors on polypharmacy (five or more meds), the risk drops even more. These services also track when pills are taken. If you skip a dose, they know. And they call.How It Works: The Step-by-Step Process
Getting started is simpler than most people think. Here’s how it typically unfolds:- Referral and assessment: Your doctor refers you to a Medicare-certified home health agency. A nurse visits your home within 48 hours to review your medications, check your health status, and talk to you about your daily routine.
- Medication reconciliation: The nurse compares your current list against hospital discharge papers, pharmacy records, and what you say you’re taking. They flag duplicates, outdated prescriptions, or conflicting drugs.
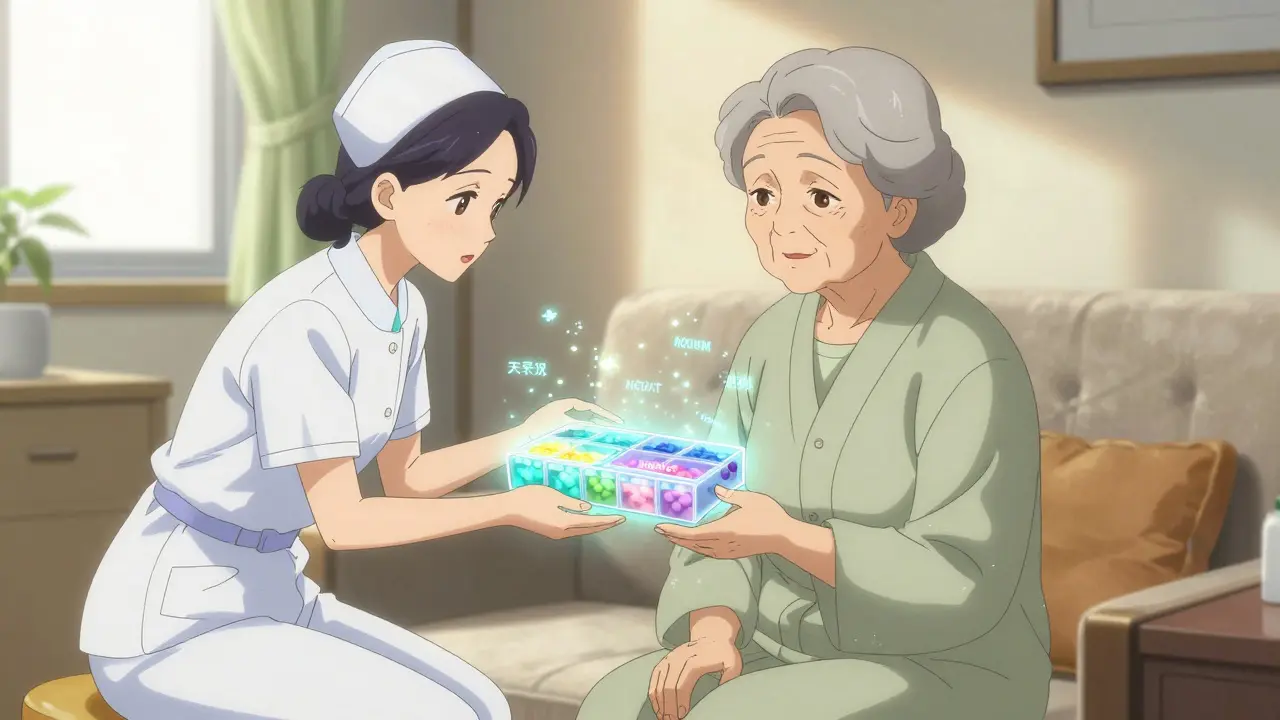
- Organization system setup: You get a personalized system. This could be a color-coded pill box, daily pouches labeled by time of day (morning, afternoon, evening), or a digital app with alarms and biometric verification.
- Training and teach-back: The nurse doesn’t assume you understand. They show you how to use the system, then ask you to explain it back in your own words. If you can’t, they try again.
- Monitoring and documentation: Each visit, the nurse checks what was taken, records it electronically, and updates your file. Any changes-new prescriptions, side effects, missed doses-are documented within 24 hours, as required by CMS guidelines.
Tools That Make a Real Difference
Technology helps, but the best tools are simple and reliable. Here’s what works:- Pill organizers: Studies show they reduce errors by up to 45%. Look for ones with compartments for morning, afternoon, evening, and bedtime. Some even lock to prevent overuse.
- Daily medication pouches: Companies like Phoenix Home Care use pre-filled, sealed pouches labeled with the date and time. You open one, take everything inside, and toss it. No counting, no confusion.
- Digital reminders: Apps with voice alerts, large buttons, and simple interfaces improve adherence by 35%. Some now include biometric checks-like a fingerprint scan-to confirm the right person took the pill.
- Visual charts: Large-print charts in your preferred language help people with vision loss or limited English. Clarest’s 2023 survey found 67% of caregivers said these charts made a big difference.

Who Qualifies and How to Get It Covered
Medicare Part A covers home health medication management-but only if you meet certain rules. You must:- Be homebound (leaving home takes great effort or medical risk)
- Need skilled nursing or therapy services
- Have a doctor’s order for home care
What It Doesn’t Do (And When It’s Not Enough)
Home health services aren’t magic. They can’t replace your doctor or pharmacist. They also struggle with certain situations:- Psychiatric medications: Drugs like antipsychotics or mood stabilizers often need frequent dose changes. Home health staff aren’t trained to adjust these. That requires a psychiatrist.
- 24/7 coverage: If you need help at 3 a.m., most agencies can’t respond. Emergency plans are essential.
- Coordination gaps: If your cardiologist, neurologist, and primary care doctor aren’t talking to each other, medication errors still happen. One Reddit user shared that inconsistent communication led to a dangerous blood thinner interaction that sent him to the ER.
Real Results: What Families Say
Mary K. from Ohio started using Phoenix Home Care’s WellPack system for her 84-year-old mother. Before, her mom missed 30% of her doses. Within two weeks, it dropped to under 5%. “It’s not just about the pills,” she said. “It’s knowing someone’s watching.” Clarest’s 2023 survey of 500 caregivers found that 78% saw better adherence with home health support. But 42% still struggled with coordinating between multiple specialists. That’s the biggest pain point: fragmented care.
What to Watch Out For
Not all agencies are the same. Here’s how to avoid trouble:- Ask about reconciliation practices: Only 65% of agencies consistently update medication lists during care transitions, even though CMS requires it. Ask: “Do you compare my list to hospital records every time I’m discharged?”
- Check documentation habits: CMS requires changes documented within 24 hours. Only 58% of agencies meet that. If you’re not getting updates, speak up.
- Confirm language access: If English isn’t your first language, ask if materials are available in your language. Phoenix Home Care now includes QR codes linking to video instructions in 17 languages.
- Watch for staffing issues: The home health nurse vacancy rate hit 28% in 2023. If visits are canceled often or staff seem rushed, it’s a red flag.
Future Trends You Should Know
The field is changing fast. By 2025, 65% of agencies are expected to use AI tools that scan your meds for dangerous interactions before you even take them. Medicare Advantage plans are starting to cover continuous monitoring devices that alert nurses if you haven’t taken your pills in 24 hours. The big win? Cost savings. Clarest’s 2023 study found that each patient using professional medication management saves about $1,200 in avoidable hospital costs per month. That’s why CMS now ties reimbursement to medication adherence rates. Agencies that fail to improve adherence face up to 8% less pay.What You Can Do Right Now
You don’t have to wait for a crisis to get help. Start today:- Write down every medication you take-include vitamins, supplements, and over-the-counter pills.
- Bring that list to your next doctor visit. Ask: “Is this still right? Are any of these duplicates or risky together?”
- Call your local Medicare-certified home health agency. Ask if they offer medication management and what the eligibility requirements are.
- Set up a simple pill organizer-even a $10 one from the pharmacy. Use meal times or bedtime as cues to take your meds.
- Teach someone in your household how to use your system. Make sure they know who to call if you miss a dose.
Medication management isn’t about control. It’s about freedom. Freedom to stay in your home. Freedom to avoid the ER. Freedom to live without the fear of a wrong pill leading to a fall, a stroke, or worse. Home health services make that possible.
Can Medicare cover home health medication management if I don’t need therapy?
Yes, but only if you’re homebound and need skilled nursing care. Medication management alone isn’t enough. You must also qualify for skilled nursing services, like wound care, injections, or monitoring for unstable conditions. If you only need help remembering to take pills without any medical supervision, Medicare won’t cover it-you’d need private pay.
What if I miss a dose? Will someone come right away?
Home health staff don’t respond to missed doses in real time. They track missed doses during scheduled visits and flag them for follow-up. If you miss a critical medication-like insulin or blood pressure pills-your family or emergency contact should call 911 or your doctor. Agencies provide emergency plans, but they’re not on-call 24/7.
Can home health nurses adjust my medication doses?
No. Nurses can report side effects or missed doses, but they cannot change your prescriptions. Only your doctor can adjust dosages. That’s why regular medication reviews with your provider are essential. Some agencies use the Beers Criteria to flag potentially inappropriate drugs for seniors, but the final decision always rests with the prescriber.
Are digital apps better than pill organizers?
It depends. Apps are great for reminders and tracking, but they require tech skills and reliable internet. For someone with memory issues or limited vision, a physical pill box with large labels and clear time slots is often more reliable. The best solution combines both: a simple organizer with a phone alarm as backup.
How often should my medication list be reviewed?
At least every 3 months, or whenever you see a new doctor or get discharged from the hospital. The American Geriatrics Society recommends regular reviews using the Beers Criteria to catch outdated or risky prescriptions. Many home health agencies do this automatically during each visit, but you should confirm it’s happening.
What if I don’t trust the home health worker?
You have the right to request a different aide or nurse. Ask the agency for a new provider. If they refuse or make you feel pressured, contact your local Area Agency on Aging or Medicare at 1-800-MEDICARE. Your safety and comfort matter. No one should be forced to accept care they don’t trust.