Brand Name Drugs: What They Are, How They Compare, and Why They Cost More
When you hear brand name drugs, the original versions of medications developed and marketed by pharmaceutical companies under a patent-protected name. Also known as originator drugs, they’re the first to hit the market after years of research and clinical trials. These are the pills you see advertised on TV, prescribed by your doctor, and often the first option your pharmacy offers. But they’re not the only option—and understanding the difference between them and generic drugs, chemically identical versions released after the patent expires can save you hundreds, even thousands, a year.
Brand name drugs carry a premium price because the company that made them had to cover the cost of discovery, testing, and marketing. That’s why a 30-day supply of a brand name statin might cost $200, while its generic version costs $10. But here’s the catch: once the patent runs out, other manufacturers can legally make the same drug with the same active ingredient, same dosage, same effect. The FDA requires generics to meet the same safety and effectiveness standards. So why do people still choose brand name? Sometimes it’s habit. Sometimes it’s fear. And sometimes, it’s because a small group of patients report subtle differences—though studies show these are rarely due to the drug itself and more likely tied to placebo effects or inactive ingredients like fillers or dyes.
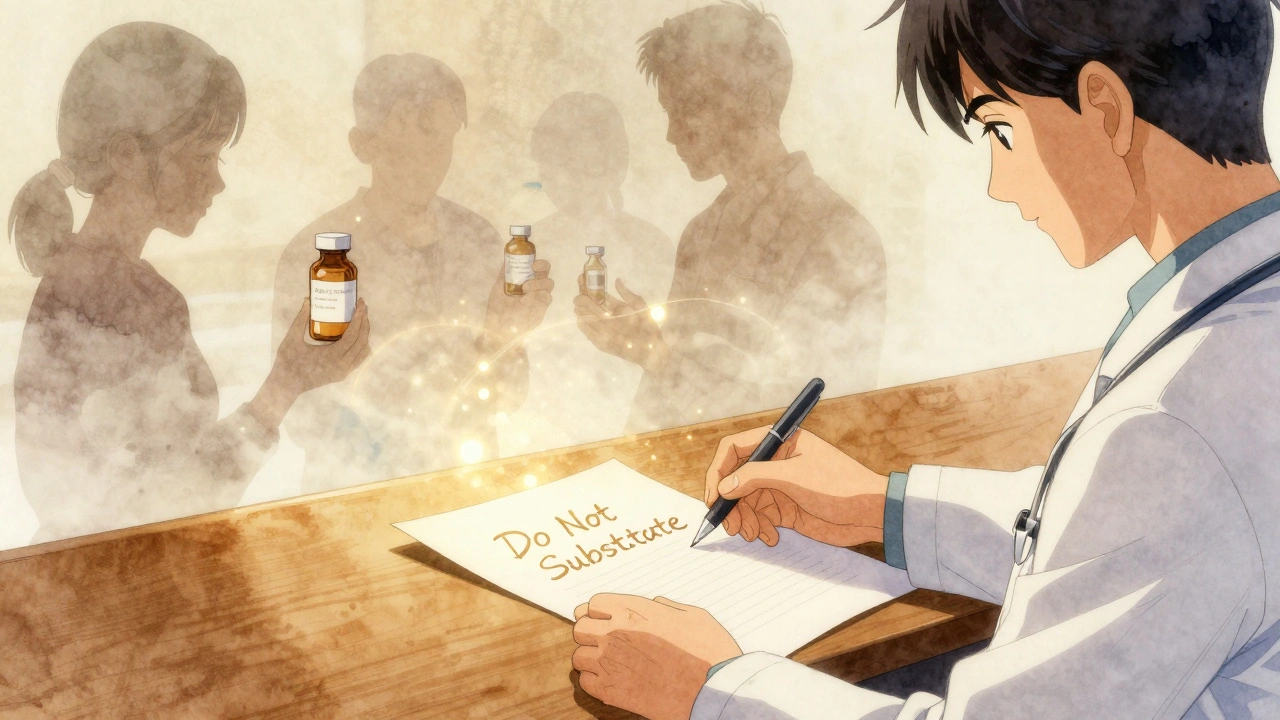
That’s where things get messy. Some drug interactions, how one medication affects another in your body can vary slightly between brand and generic due to different inactive components, especially in sensitive populations like the elderly or those with kidney or liver issues. For example, if you’re on lithium, a mood stabilizer used for bipolar disorder that has a narrow safety window, even tiny changes in absorption can push levels into toxic territory. That’s why some doctors stick with brand name for high-risk meds—even if it’s not always necessary.
And then there’s the bigger picture: how government policies, patent extensions, and market monopolies keep prices high. In the U.S., drug companies can tweak a formula just enough to get a new patent—this is called evergreening—and it keeps generics off the market longer. Meanwhile, countries like Australia and the UK use systems like the Pharmaceutical Benefits Scheme, a government program that negotiates prices and subsidizes medications for citizens to keep costs down. The result? Americans pay more for the same pills.
What you’ll find in the posts below isn’t just a list of drugs. It’s a look at how brand name drugs fit into real-world medicine: how they interact with other meds, how side effects show up differently across populations, how insurance and pricing shape choices, and when sticking with the original brand actually matters. You’ll see how REMS programs, FDA safety plans for high-risk medications sometimes target brand name drugs specifically, why some patients need to track side effect tracking, the process of recording symptoms to identify medication triggers carefully, and how even something as simple as a pill’s shape or color can affect how people take—or refuse—medication.
There’s no one-size-fits-all answer. But knowing the facts helps you ask the right questions—of your doctor, your pharmacist, and your insurance company. You don’t have to accept the first price you’re given. You don’t have to take the first pill they hand you. And you definitely don’t have to pay more than you need to.