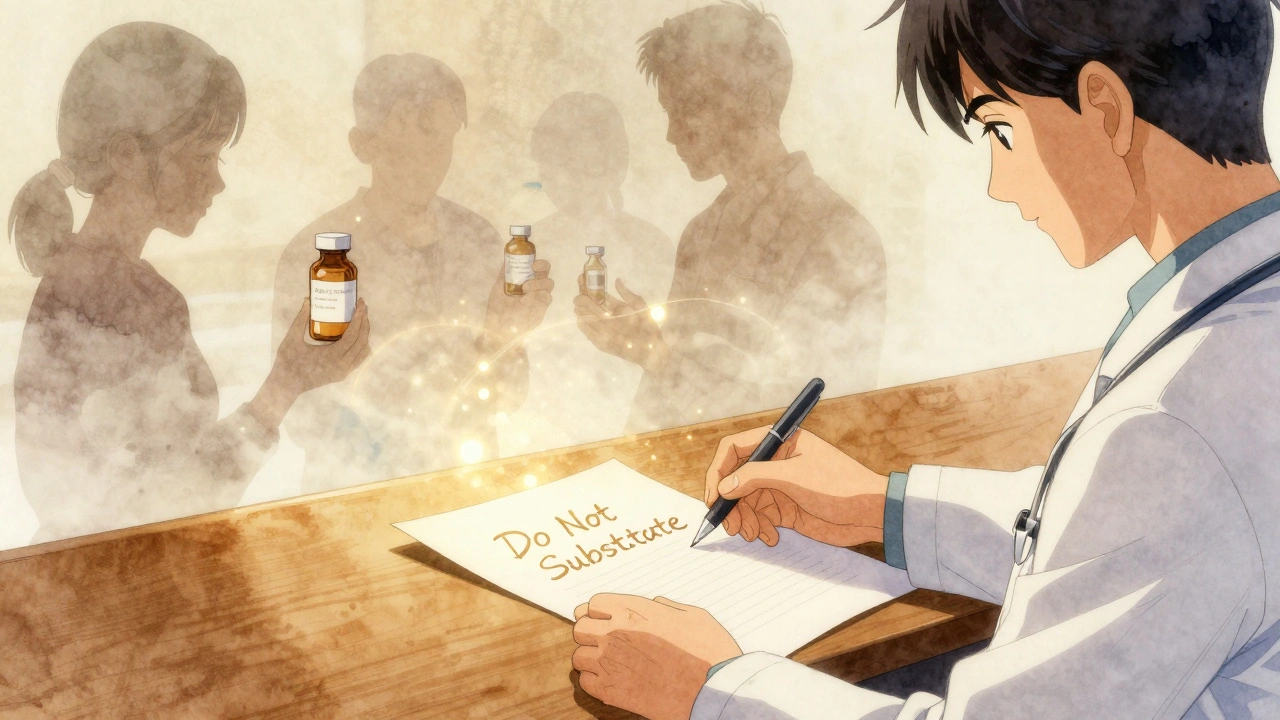
Most of the time, when you get a prescription, your pharmacist automatically swaps the brand-name drug for a cheaper generic. It’s legal, safe, and saves you money-often hundreds of dollars a month. But sometimes, your doctor writes "Do Not Substitute" on the prescription. And that changes everything.
What Does "Do Not Substitute" Actually Mean?
"Do Not Substitute" (also called DAW, or "Dispense as Written") is a clear instruction from your doctor telling the pharmacist: give me exactly what I wrote on this paper-no generics allowed. This isn’t just a suggestion. It’s a legally binding directive in every U.S. state. Pharmacies are required to follow it, even if the generic is cheaper, covered better by insurance, or even preferred by the patient.This rule exists because, while most generics work just as well as brand-name drugs, there are some cases where the difference matters. Not because generics are bad-they’re not. But because some medicines are so sensitive that even tiny changes in how they’re made can affect how your body responds.
When Is a Brand Drug Really Necessary?
Not every prescription needs to be brand-only. In fact, 90% of all prescriptions filled in the U.S. are for generics. But for certain drugs, switching can be risky. The FDA calls these narrow therapeutic index (NTID) drugs. These are medications where the difference between a helpful dose and a dangerous one is very small.Examples include:
- Levothyroxine (for thyroid conditions): Even a 5% change in absorption can throw your hormone levels off, leading to fatigue, weight gain, or heart problems.
- Warfarin (a blood thinner): A small variation in how your body processes the drug can mean the difference between preventing a clot and causing a bleed.
- Phenytoin (for seizures): If levels drop too low, seizures can return. If they rise too high, you risk toxicity.
A 2021 study from the FDA’s adverse event database found over 1,200 cases where patients had serious health issues after switching from brand to generic versions of these drugs. That’s not common-but it’s enough to justify caution.
Other reasons doctors use "Do Not Substitute" include:
- Patients who had a bad reaction to a generic version (like an allergic response to a filler or dye).
- Complex drug delivery systems, like inhalers or prefilled pens, where the generic might look the same but doesn’t work the same way.
- Biologic drugs (like Humira or Enbrel), which are made from living cells. Even if a biosimilar is approved, the FDA requires special "interchangeable" status before substitution is allowed-and only 12 have achieved that so far.
How Do Doctors Make This Call?
It’s not arbitrary. In most states, the law requires doctors to write something specific on the prescription. Common phrases include:- "Do Not Substitute"
- "Dispense as Written"
- "DAW"
- "Medically Necessary"
In some states, like New York, you also need the doctor’s initials next to the note. In California, electronic prescriptions use checkboxes. If the instruction isn’t written correctly, the pharmacy can legally substitute the generic-even if the doctor meant otherwise.
Doctors aren’t supposed to use "Do Not Substitute" just because they prefer the brand. The American College of Physicians says inappropriate use of DNS prescriptions adds $15.7 billion in unnecessary costs to the U.S. healthcare system each year. That’s why many doctors now document the reason clearly in the patient’s chart: "Patient had seizure recurrence after switching from brand to generic phenytoin," or "Thyroid levels unstable after generic levothyroxine switch."

Why Are Some Patients Shocked by the Cost?
Many people don’t realize how big the price difference is. A brand-name drug like Synthroid can cost $85 for a 30-day supply. The generic? $10. That’s an 88% drop.A 2022 Kaiser Family Foundation survey found that 68% of patients who got a "Do Not Substitute" prescription didn’t know they’d be charged significantly more until they got to the pharmacy counter. That’s a problem.
One Reddit user wrote: "My doctor wrote DAW on my Synthroid script. I thought it was just a formality. My insurance charged me $85. I had to call my doctor’s office just to find out why they wouldn’t let me get the $10 version."
Doctors aren’t always aware of the financial impact. Some use "Do Not Substitute" out of habit, or because they were taught to stick with the brand they’re familiar with. But experts like Dr. Aaron Kesselheim from Harvard say: "We’re seeing DNS rates of 25-30% in some drug classes where there’s zero clinical reason to avoid generics. That’s not medicine-it’s inertia."
What Happens When the Pharmacy Can’t Fill It?
Even with a "Do Not Substitute" order, things can go wrong. Insurance companies sometimes reject the claim because they think it’s unnecessary. Pharmacists might call the doctor’s office to double-check. In one survey, 73% of community pharmacists said insurance systems incorrectly block DNS prescriptions 15-20% of the time.If this happens, you have options:
- Ask the pharmacist to call the doctor’s office and confirm the DAW order.
- Ask if the doctor can write a letter of medical necessity to your insurance.
- If the drug is a biologic, ask if an FDA-approved interchangeable biosimilar is available.
Electronic health record systems like Epic often default to generic substitution. That means doctors have to manually override the system every time they want to block it. One Johns Hopkins study found it takes an average of 2.3 minutes per prescription to properly document a DNS order. For a doctor seeing 50 patients a day, that’s almost two extra hours of work.

What’s Changing Right Now?
The rules around generics and brand drugs are evolving. The FDA is investing $50 million over the next five years to improve testing for narrow therapeutic index drugs. The goal? To prove that even these sensitive medications can be safely switched-so fewer patients need brand-only prescriptions.At the same time, 18 states passed new laws in 2023 to limit "Do Not Substitute" orders to only those cases with documented medical need. Seven states now require prior authorization from insurers before allowing brand-name drugs when a generic exists.
And Medicare, which covers over 60 million Americans, will start tracking DNS usage closely starting in 2024. The idea? To identify patterns of overuse and reduce waste.
Experts predict that by 2027, DNS rates for small-molecule drugs (like levothyroxine or warfarin) will drop from 8-12% to just 5-7%. But for biologics-complex drugs made from living cells-DNS will likely stay above 50%, simply because the science isn’t there yet to prove safe switching.
What Should You Do?
If you get a "Do Not Substitute" prescription:- Ask your doctor: "Why am I getting the brand? Is there a specific reason?"
- Ask your pharmacist: "Is there a cheaper generic or interchangeable biosimilar available?"
- Check your insurance statement. If you’re paying $80 for a drug that costs $10 as a generic, you may be eligible for a patient assistance program.
- If you’ve had a bad reaction to a generic in the past, tell your doctor and pharmacist-keep a record.
Don’t assume your doctor is trying to charge you more. Many don’t even know the cost difference. But don’t assume the generic is always safe, either. For some people, the brand is the only thing that works.
The goal isn’t to ban generics. It’s to make sure that when a patient needs the brand, they get it-without unnecessary cost or confusion.
Can a pharmacist refuse to fill a "Do Not Substitute" prescription?
No. Pharmacists are legally required to follow a "Do Not Substitute" order. If they don’t, they risk losing their license. However, they can call the doctor to confirm the order if they suspect a mistake or if insurance denies payment.
Are generic drugs always safe?
Yes-for 99.5% of drugs, generics are just as safe and effective as brand-name versions. The FDA requires them to have the same active ingredient, strength, dosage form, and route of administration. But for a small group of drugs called narrow therapeutic index (NTID) medications, even tiny differences in how they’re absorbed can cause problems. That’s why DNS exists.
Why are biologics treated differently than other generics?
Biologics are made from living cells, not chemicals. This makes them far more complex than traditional pills. A generic version of a biologic is called a biosimilar, and it’s not automatically interchangeable. The FDA must approve it as "interchangeable"-meaning it can be swapped without risk. Only 12 have achieved this status as of late 2023. Until then, "Do Not Substitute" is standard.
Can I ask my doctor to switch from brand to generic if I’m on a "Do Not Substitute" prescription?
Yes. If you’re concerned about cost or want to try a generic, talk to your doctor. They can review your medical history and decide if switching is safe. For drugs like levothyroxine or warfarin, they may agree to a trial under close monitoring.
Does "Do Not Substitute" mean the brand is better?
No. It doesn’t mean the brand is stronger, more effective, or higher quality. It means that for your specific condition, switching could be risky. For most people, the generic is just as good. For a small number, the brand is the only safe option.
How can I find out if my drug has a generic version?
Ask your pharmacist or check the FDA’s Orange Book, which lists all approved drugs and their generic equivalents. You can also search online using the drug’s generic name. If it’s listed as "AB-rated," it’s considered therapeutically equivalent.