CMS Patient Safety Measures: Key Protocols to Prevent Medication Errors and Harm
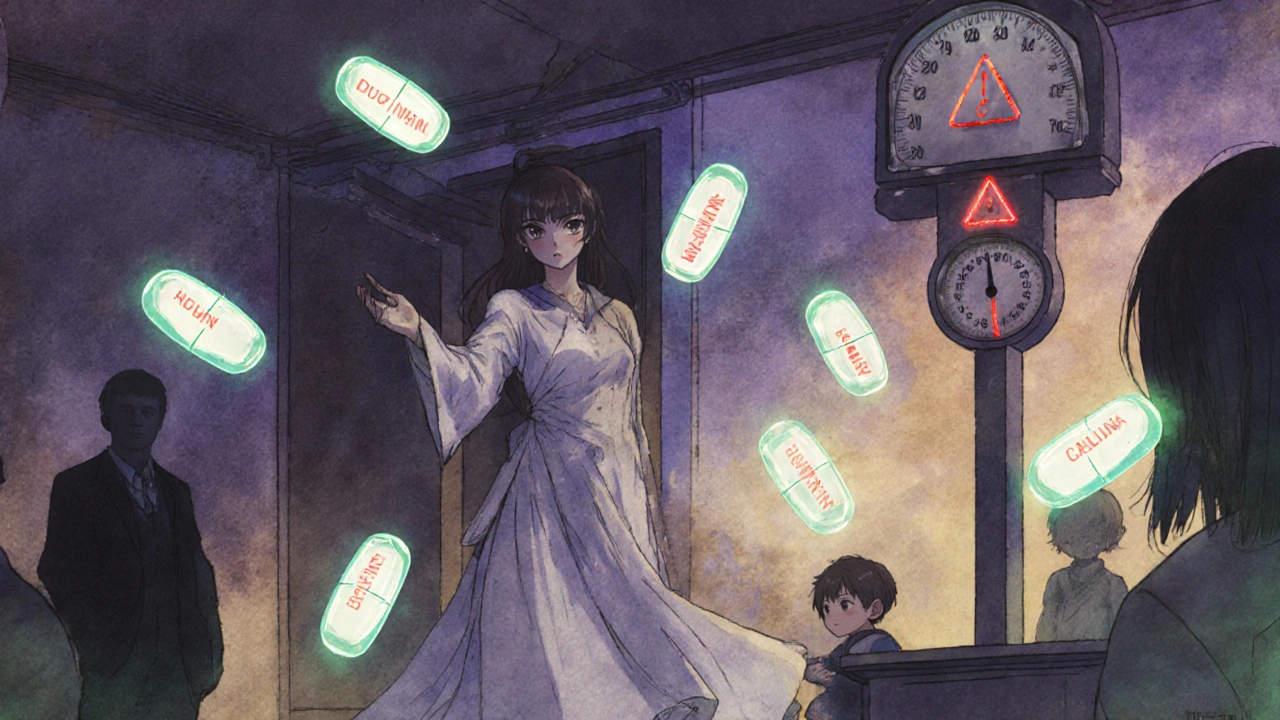
When hospitals and clinics follow CMS Patient Safety Measures, a set of federal guidelines designed to reduce preventable harm in healthcare settings. Also known as Medicare safety standards, these rules aren’t just paperwork—they’re the reason you don’t get the wrong drug, the wrong dose, or a dangerous combo like warfarin and ibuprofen when you’re not supposed to. These measures exist because mistakes happen. Too often. And they don’t just cause discomfort—they kill.
One of the biggest dangers? drug interactions, when two or more medications clash in harmful ways. For example, combining warfarin with NSAIDs like naproxen can spike your bleeding risk by up to four times. That’s not a theory—it’s a documented outcome tracked under CMS safety reporting. Same goes for antibiotic photosensitivity, a reaction where drugs like doxycycline or TMP-SMX turn your skin into a sunburn magnet. Bactrim isn’t just a pill—it’s a potential burn risk if you’re not warned. CMS requires providers to document these risks clearly, yet too many patients still get caught off guard.
Then there’s medication adherence, how consistently patients take their drugs as prescribed. Dolutegravir for HIV or vidagliptin for diabetes only work if you don’t skip doses. CMS tracks non-adherence as a safety failure because missed pills lead to hospitalizations, resistance, and worse outcomes. That’s why safety protocols now push for simpler regimens, pill organizers, and follow-ups—not just prescriptions.
And it’s not just about pills. skin reactions, like the rare but terrifying AGEP rash triggered by meds, are now flagged as critical safety events. If a patient breaks out in pustules after starting a new drug, stopping that drug fast is part of the protocol. Same with butenafine cream—skin irritation might seem minor, but if it’s ignored, it can turn into a full-blown allergic crisis. CMS expects providers to recognize these early signs and act.
Even something as simple as what you wear matters. fungal skin infections, like yeast rashes worsened by tight, non-breathable fabrics, are preventable with basic advice. CMS encourages staff to educate patients on clothing choices because infection control isn’t just about hand sanitizer—it’s about daily habits. And when it comes to older adults, iron deficiency anemia, often missed because symptoms look like normal aging, is now a targeted safety concern. Low ferritin isn’t just a lab result—it’s a sign of underlying neglect if not checked.
The posts below don’t just list drugs. They show you the real-world risks behind the safety rules. You’ll see how CMS Patient Safety Measures connect to everything from ear drops and inhalers to cholesterol pills and antiparasitics. No theory. No fluff. Just what happens when protocols work—and what goes wrong when they don’t. These are the stories behind the guidelines. And they’re the ones that keep you alive.