When choosing birth control, it’s not just about convenience-it’s about safety. The contraceptive patch, vaginal ring, and IUD are all effective, but they carry very different risks. If you’ve ever wondered which one is safest for your body, you’re not alone. Many women switch methods because of side effects they didn’t expect. Some end up with blood clots. Others get heavier periods than ever. The truth? Not all hormonal birth control is created equal. And IUDs, especially, are quietly becoming the top choice for women who want long-term protection without the hidden dangers.
How the Patch, Ring, and IUD Work
The patch (Xulane®) sticks to your skin and releases hormones-norelgestromin and ethinyl estradiol-straight into your bloodstream. You change it every week for three weeks, then take a break. The vaginal ring (NuvaRing®) works similarly but sits inside your vagina. It releases etonogestrel and ethinyl estradiol daily and stays in for three weeks. Both methods deliver estrogen, which increases your risk of blood clots.
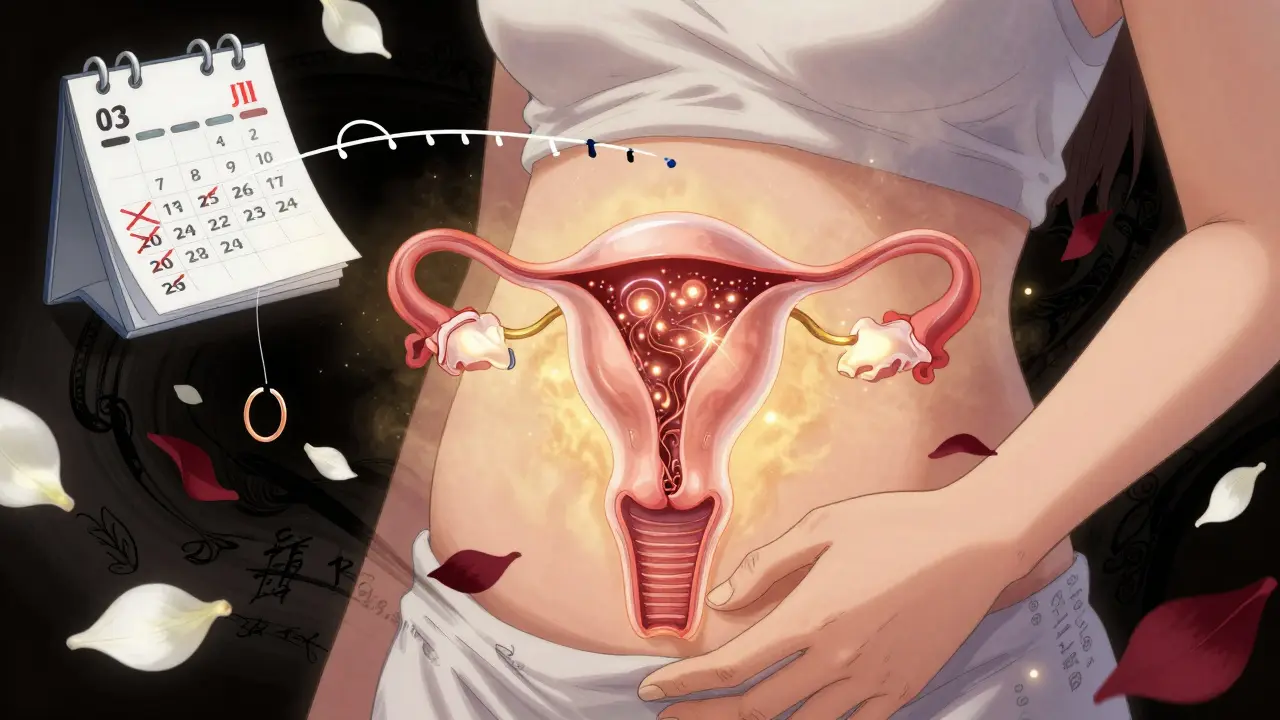
IUDs are completely different. The copper IUD (Paragard®) doesn’t use hormones at all. It releases copper ions that make your uterus toxic to sperm. Hormonal IUDs like Mirena®, Liletta®, and Kyleena® release small amounts of levonorgestrel directly into the uterus. This thickens cervical mucus and thins the lining, preventing pregnancy. No estrogen. No daily pills. No weekly patches.
That difference in delivery matters. The patch and ring send hormones through your whole body. IUDs work locally. That’s why their side effect profiles are so different.
Blood Clot Risk: Patch vs. Ring vs. IUD
Estrogen is the problem. It raises your chance of dangerous blood clots in your legs or lungs. For healthy women under 35 who don’t smoke, the risk is still low-about 7 to 10 cases per 10,000 women per year with estrogen-containing methods. But here’s the catch: the patch delivers more estrogen than the pill or ring. A 2022 JAMA review confirmed women using the patch have a higher clot risk than those on oral contraceptives, even though both contain estrogen.
The ring? It’s slightly better than the patch, but still carries the same clot risk as the pill. If you have migraines with aura, high blood pressure, or a history of clots, you should avoid both.
Now, compare that to IUDs. Copper IUDs have zero estrogen. Hormonal IUDs release progestin only-no estrogen at all. That means their clot risk is nearly the same as not using birth control. The American College of Obstetricians and Gynecologists (ACOG) recommends IUDs as first-line birth control for most women because of this exact reason. If you’re worried about blood clots, an IUD isn’t just safer-it’s the safest option among these three.
Effectiveness: Why IUDs Win
Perfect use? All three methods are over 99% effective. But real life isn’t perfect. People forget to change the patch. The ring slips out. You leave it in too long. That’s where failure rates tell the real story.
Typical use failure rates:
- Contraceptive patch: 9% (91% effective)
- Vaginal ring: 7% (93% effective)
- Hormonal IUD: 0.2% (99.8% effective)
- Copper IUD: 0.8% (99.2% effective)
That’s not a small difference. For every 100 women using the patch or ring for a year, about 7 to 9 will get pregnant. With an IUD, it’s less than one. A 2022 study in JAMA Network Open found that short-acting methods like the patch and ring had pregnancy rates over 4.5 per 100 women-years. IUDs? Just 0.27. That’s why doctors call IUDs “set it and forget it.” You don’t have to remember anything. No weekly reminders. No monthly insertions. Just long-term protection.
Safety Risks: What to Expect
Let’s break down the common side effects and rare but serious risks for each method.
Contraceptive Patch
- Common: Skin irritation (42% of users), breakthrough bleeding (37%), nausea
- Rare but serious: Blood clots, stroke, heart attack (higher than pill users)
- Practical issue: Patches can fall off. About 1.8% completely detach; 2.8% partially detach. If it’s off for more than 24 hours, you’re not protected.
Vaginal Ring
- Common: Vaginal discomfort (38%), increased discharge, breakthrough bleeding
- Rare but serious: Blood clots (similar to pill), expulsion during sex (3-5% of users)
- Practical issue: If it slips out, you have to rinse and reinsert within 3 hours. If it’s out longer, you need backup contraception.
IUDs
- Copper IUD (Paragard®): Heavier periods (57% of users), worse cramps, spotting between periods
- Hormonal IUD (Mirena®, Liletta®, etc.): Irregular bleeding at first (improves after 6-12 months), lighter periods or no periods at all (30-50% of users)
- Shared risks: Expulsion (2-10%), uterine perforation (0.1-0.6%), infection (1-2% in first 20 days after insertion)
- Important: IUDs don’t raise clot risk. They may even lower your risk of endometrial cancer.
One user on Reddit switched from NuvaRing to Mirena after three months of severe migraines. She realized the estrogen in the ring was triggering them. Another user had Paragard for two years-her periods became unbearable. She switched to Liletta and now has just two days of light spotting. These aren’t rare stories. They’re common.

Who Should Avoid Each Method?
Not everyone can use every method. Here’s who should skip what:
- Avoid the patch and ring if you: Smoke and are over 35, have migraines with aura, have a history of blood clots, have uncontrolled high blood pressure, or have liver disease.
- Avoid IUDs if you: Have untreated STIs, have certain uterine abnormalities (like a severely distorted uterus), or have had a pelvic infection in the last 3 months.
Also, if you’ve never had a baby, some doctors still hesitate to recommend IUDs. But ACOG says that’s outdated. IUDs are safe for people who’ve never given birth. The biggest barrier? Fear of pain during insertion. Yes, it hurts-like strong menstrual cramps. But it’s over in minutes. Most people say it’s worth it.
Cost and Accessibility
Cost matters. The patch costs $15 to $80 a month without insurance. The ring is $0 to $200. IUDs? Upfront cost is $0 to $1,300. But here’s the trick: IUDs last 3 to 12 years. That’s less than $10 a month over time. Many insurance plans cover them fully under the Affordable Care Act. Planned Parenthood and community clinics often offer sliding scale fees.
And if you need emergency contraception? The copper IUD is the most effective option. Inserted within 120 hours of unprotected sex, it reduces pregnancy risk to just 0.1%. No other method comes close.
Real User Experiences
Let’s look at what real people say:
- Patch (Healthgrades): 3.2/5 rating. 42% had skin irritation. 37% had breakthrough bleeding.
- Ring (Drugs.com): 3.6/5. 45% loved the convenience. 38% had discomfort or expulsion.
- Hormonal IUD (Mirena®): 3.9/5. 68% had lighter periods. 32% had irregular bleeding at first.
- Copper IUD (Paragard®): 3.5/5. 57% said periods got worse. But 43% said they’d choose it again.
One study found 20% of patch users quit within six months. For copper IUDs? Only 9% stopped. That’s not about willpower. It’s about side effects. If your body doesn’t like the hormones, you’ll notice. If your body reacts to copper, you’ll notice. But if you find the right fit, you’ll stick with it.
What Experts Say
Dr. Jen Gunter, OB/GYN and author of The Vagina Bible, says: “IUDs have the lowest failure rate of any reversible method and don’t carry the blood clot risks associated with estrogen-containing methods.”
The Cleveland Clinic confirms IUDs reduce endometrial cancer risk. The FDA has issued warnings about the patch’s higher clot risk compared to pills. And the Contraceptive CHOICE Project showed that when cost and access aren’t barriers, 75% of women choose IUDs-and unintended pregnancies drop dramatically.
Dr. Sarah Prager from the University of Washington puts it simply: “The best birth control is the one that works for the individual’s body, lifestyle, and risk factors.”
Switching Methods: What You Need to Know
If you’re switching from one method to another, timing matters. You can’t just stop the ring and slap on a patch. Hormones overlap. You could get breakthrough bleeding or even ovulate. Always use backup contraception for 7 days when switching between hormonal methods. If you’re switching from a hormonal IUD to the patch, wait until the IUD is removed before starting. Don’t try to combine them.
Copper IUDs work immediately. If you need emergency contraception, it’s the best option. Hormonal methods take 7 days to become effective if started mid-cycle.
Final Thoughts: Which One Is Right for You?
If you want the safest, most effective, and lowest-maintenance option-go with an IUD. Copper if you want no hormones. Hormonal if you want lighter periods and less cramping. The patch and ring are fine if you’re young, healthy, don’t smoke, and can remember to change them on time. But if you’ve ever missed a pill, forgot to change your patch, or had the ring fall out, you know how easy it is to slip up.
IUDs don’t care if you’re busy, forgetful, or stressed. They just work. And they don’t raise your risk of clots. That’s why they’re becoming the gold standard.
Before you choose, talk to your provider. Bring your medical history. Ask about your personal risk for blood clots. Ask about your period preferences. Ask what happens if you change your mind. The right method isn’t the one everyone else uses. It’s the one that fits your life-and keeps you safe.
Is the contraceptive patch safer than the ring?
Neither is truly safer. Both contain estrogen and raise the risk of blood clots. Studies show the patch delivers more estrogen than the ring, which may make clot risk slightly higher. The ring is easier to manage if you forget to change things weekly, but both require consistent use. If you’re concerned about clots, an IUD is the better choice.
Can IUDs cause infertility?
No. IUDs do not cause infertility. This is a common myth. Once removed, fertility returns to normal within a month. Infection is the only risk that could affect fertility-and that’s rare, happening in just 1-2% of cases within the first 20 days after insertion. Proper screening for STIs before insertion reduces this risk even further.
Do hormonal IUDs cause weight gain?
Most studies show no significant weight gain from hormonal IUDs. Some users report bloating or water retention early on, but this usually fades. Unlike the pill or patch, hormonal IUDs don’t flood your whole body with hormones-they work locally. Weight gain is more likely linked to diet, stress, or other factors than the IUD itself.
How painful is IUD insertion?
It varies. Some people feel mild cramping. Others describe it as strong period cramps that last a few minutes. Most find it manageable. Taking ibuprofen an hour before helps. Some providers offer local numbing. The discomfort is brief, and most people say the benefits far outweigh the momentary pain.
Can I use the ring if I have migraines?
If you have migraines with aura, you should avoid the ring. Estrogen in the ring can trigger severe headaches or increase stroke risk. Even if your migraines are mild, estrogen can make them worse. Switching to a progestin-only method like an IUD or implant is safer. Talk to your doctor before continuing.
Is the copper IUD bad for your body?
It’s not bad-it’s just different. Copper IUDs cause heavier, longer periods and stronger cramps for many users. But they’re hormone-free, which makes them ideal for people who can’t or won’t take hormones. They’re also the most effective form of emergency contraception. If you’re okay with heavier bleeding, it’s one of the safest long-term birth control options.
How long does it take for the patch to start working?
If you start the patch on the first day of your period, it works immediately. If you start later, you need to use backup contraception (like condoms) for the first 7 days. Always follow your provider’s instructions-timing matters.
Can IUDs move or fall out?
Yes, but it’s rare. Expulsion happens in 2-10% of cases, usually in the first few months. Signs include feeling the strings lower than usual or not feeling them at all. If you suspect expulsion, use backup contraception and see your provider. Uterine perforation is even rarer-less than 1 in 1,000 insertions.

