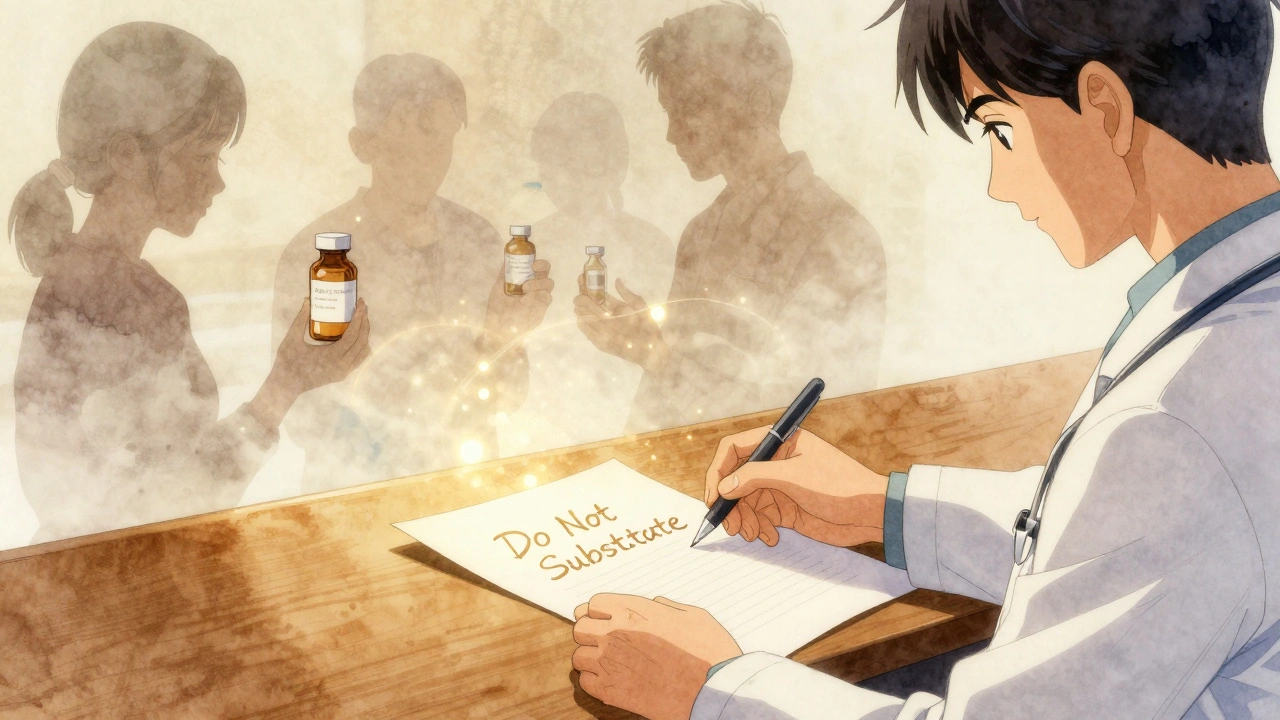
Do Not Substitute: Why Changing Medications Can Be Dangerous
When a pharmacist hands you a different pill with the same name, it’s easy to assume it’s just a cheaper version of the same thing. But do not substitute, a critical warning on prescriptions that means swapping drugs can lead to life-threatening reactions, reduced effectiveness, or hidden side effects. This isn’t just about brand vs. generic—it’s about how your body reacts to specific formulations, inactive ingredients, or hidden interactions that most people never think to ask about. Many patients don’t realize that even two pills labeled "simvastatin" can behave differently in their system if one has a different coating, filler, or release mechanism. That’s why drug interactions, when two or more medications affect each other’s absorption, metabolism, or effect in the body can sneak up on you. For example, switching from one statin to another might seem harmless, but if you’re also taking an antifungal or a common acid reducer like famotidine, the new version could push your liver enzymes into dangerous territory. The same goes for lithium—changing brands or switching to a generic without monitoring blood levels can trigger toxicity, even if the dose stays the same.
prescription safety, the practice of ensuring medications are taken exactly as intended, without unintended changes isn’t just about following directions. It’s about understanding that your body is a unique system. A pill that works perfectly for your neighbor might cause seizures, extreme dizziness, or kidney stress in you because of how your genes process it. That’s why generic drugs, medications approved as equivalent to brand-name versions but sometimes differing in inactive ingredients or manufacturing aren’t always interchangeable in practice. The FDA says they’re bioequivalent, but real-world data shows some patients have worse side effects or reduced control of conditions like epilepsy, thyroid disorders, or bipolar disease after a switch. In Australia, 84% of prescriptions are filled with generics—but that doesn’t mean every substitution is safe. In the U.S., some patients report sudden spikes in blood pressure or unexplained rashes after a pharmacy change. And when you’re on warfarin, even a tiny shift in how your body absorbs the drug can mean the difference between clotting and bleeding out.
Doctors and pharmacists don’t always catch these risks because they’re trained to trust labels, not individual responses. But if you’ve ever felt "off" after a refill, or noticed new symptoms after a switch, you’re not imagining it. The posts below cover real cases where medication substitution led to hospital visits: how H2 blockers can ruin antiviral treatment, why antibiotics like fluoroquinolones can trigger muscle weakness in people with myasthenia gravis, and how switching cholesterol drugs without monitoring can backfire. You’ll also find guides on reading prescription stickers, spotting dangerous interactions, and what to say when a pharmacist tries to swap your meds. This isn’t about fear—it’s about knowing your body well enough to ask the right questions before you swallow that new pill.