Understanding Gout Risk: Causes, Prevention, and Management
When dealing with gout risk, the chance of developing painful joint inflammation caused by uric acid crystal buildup. Also known as hyperuricemia complications, it affects millions worldwide and can be managed with lifestyle tweaks and medication.
Key Factors Influencing Gout Risk
At the heart of the problem lies uric acid. This waste product forms when the body breaks down purines—natural substances found in many foods and in our cells. When production outpaces elimination, uric acid spikes, eventually crystallizing in joints. The body’s ability to flush out uric acid hinges on kidney function. Poor filtration or dehydration lets levels climb, directly increasing gout risk. Genetics also play a role; some people inherit enzymes that process purines less efficiently, making them more vulnerable.
Diet is an everyday lever you can pull. Purine‑rich foods such as red meat, organ meats, shellfish, and certain legumes raise uric acid production. Even sugary drinks and high‑fructose corn syrup accelerate the process by prompting the liver to produce more purines. Swapping these for low‑purine options—like dairy, most fruits, and whole grains—helps keep levels in check. Moderation, not elimination, is the goal; occasional indulgence won’t wreck your progress if the overall diet stays balanced.
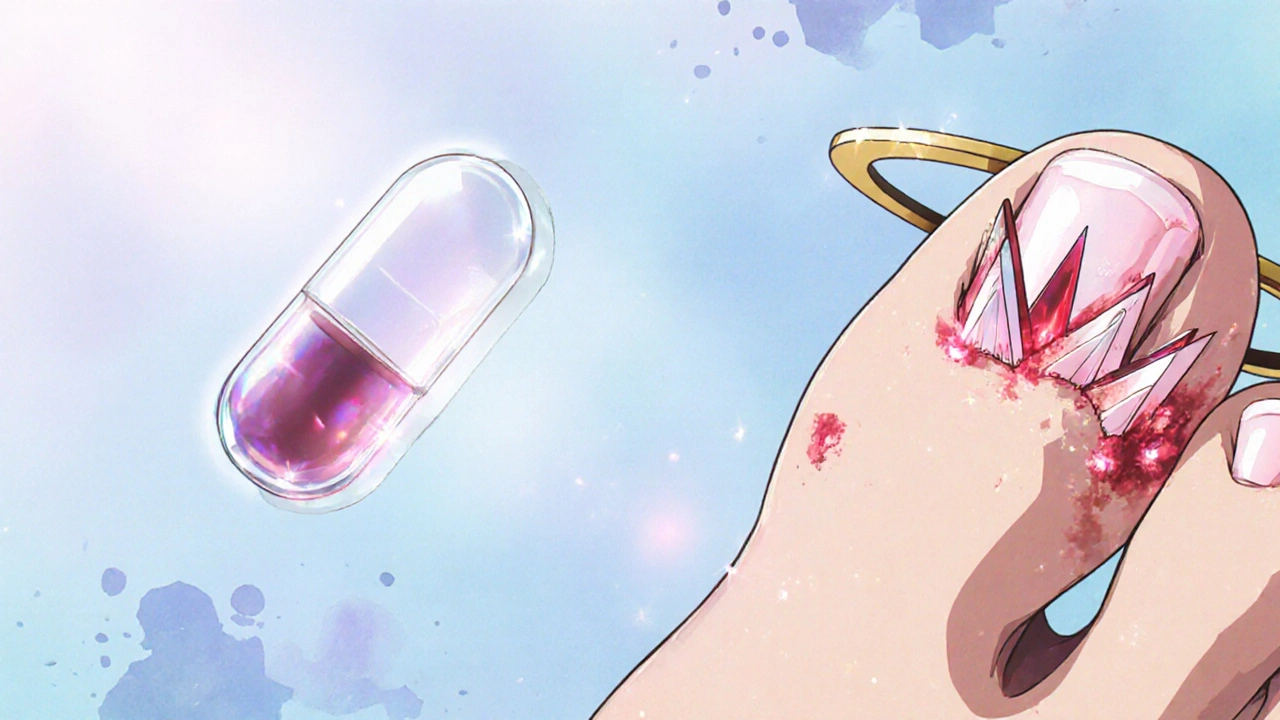
When diet alone isn’t enough, medication steps in. Drugs like allopurinol or febuxostat target the enzyme xanthine oxidase, curbing uric acid synthesis. Others, such as probenecid, boost kidney excretion. Choosing the right drug depends on factors like kidney health, existing heart disease, and drug interactions. Regular blood tests monitor uric acid levels and guide dosage adjustments, ensuring the treatment stays effective without causing side effects.
Beyond food and meds, everyday habits shape your odds. Maintaining a healthy weight reduces pressure on joints and lowers uric acid production. Alcohol, especially beer, raises uric acid and hampers kidney clearance, so limiting intake makes a big difference. Staying well‑hydrated dilutes the blood, helping kidneys flush out excess uric acid more efficiently. Simple moves—like walking instead of driving short distances—add up to lower inflammation and better overall health.
Gout rarely shows up in isolation. It often coexists with hypertension, diabetes, and metabolic syndrome, each of which can worsen uric acid handling. Managing these conditions with proper medication, diet, and exercise creates a supportive environment that further reduces gout medication needs and flares. Coordinated care among your primary doctor, rheumatologist, and nutritionist ensures all the pieces fit together.
Below you’ll find a curated set of articles that dive deeper into each of these areas—from detailed medication comparisons to practical diet guides and lifestyle tips. Use them to build a personalized plan that tackles the root causes of gout and keeps you moving pain‑free.