Ischemia: recognize, act, and reduce risk
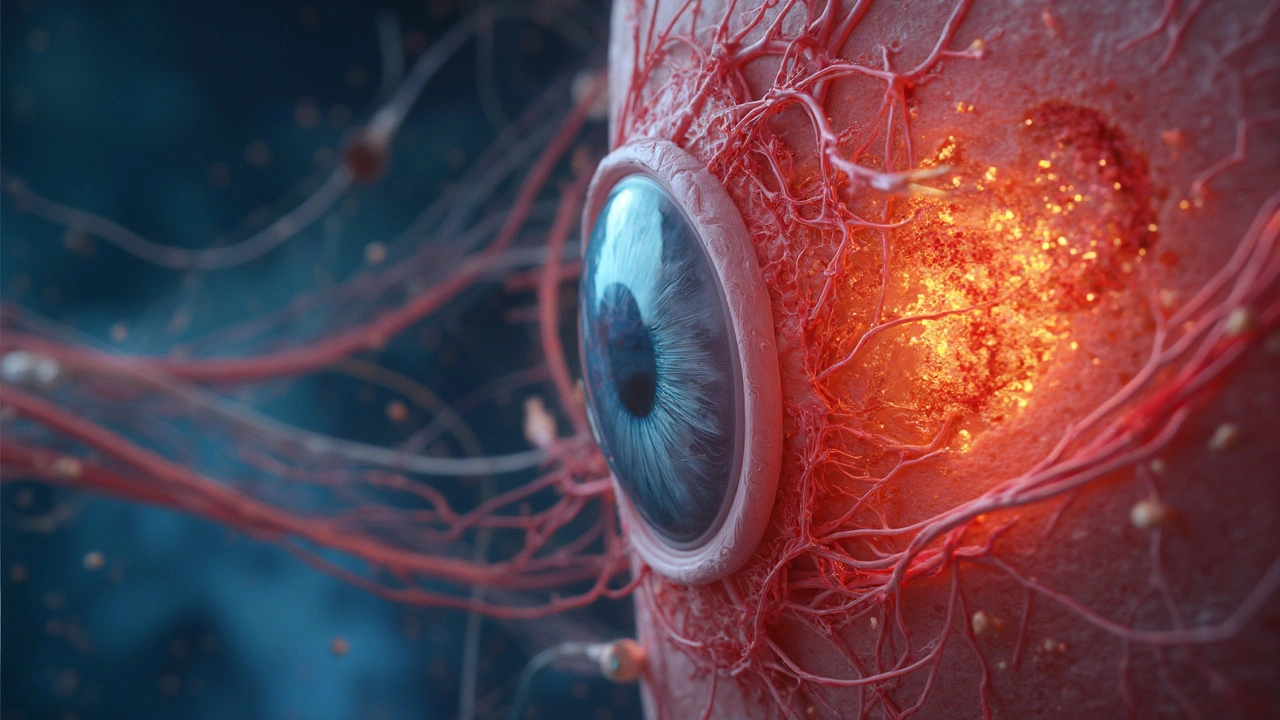
Ischemia happens when a part of your body doesn’t get enough blood and oxygen. When that occurs quickly - like during a heart attack or stroke - minutes matter. Slower, chronic ischemia shows up as pain with activity or poor wound healing. Knowing what to watch for can prevent real harm.
Common causes include blocked arteries from plaque, a sudden clot, or low blood pressure that leaves tissues starved. Myocardial ischemia affects the heart, cerebral ischemia affects the brain, and peripheral ischemia affects arms or legs. Each has different signs, but all come from the same basic problem: reduced blood flow.
How to spot ischemia
Chest pain or pressure, shortness of breath, sweating, or nausea can be heart ischemia. For the brain, sudden weakness on one side, confusion, trouble speaking, or vision loss may mean a stroke. In the legs you might notice cramping when walking, coldness, or wounds that won't heal. If symptoms start suddenly or are severe, call emergency services right away.
Doctors use tests to confirm ischemia. An ECG, cardiac enzymes, and stress tests check the heart. CT or MRI scans and carotid ultrasound check the brain and neck arteries. Ankle-brachial index and arterial Doppler help evaluate limb blood flow. These tests show where blood flow is limited and guide treatment choices.
Treatment and prevention
Immediate treatment depends on the type and urgency. For heart attacks, quick clot-busting drugs or urgent angioplasty to open the blocked artery save heart muscle. For ischemic stroke, clot-busting IV drugs or mechanical thrombectomy can restore brain blood flow if given fast. Peripheral ischemia may need angioplasty, bypass surgery, or blood-thinning medicines.
Long-term care focuses on fixing the cause and cutting risk. That means antiplatelet drugs like aspirin or clopidogrel, cholesterol-lowering statins, blood pressure control, and diabetes management. Smoking stops blood vessels from healing, so quitting is one of the strongest moves you can make. Regular exercise, a balanced diet, and steady weight control lower the chance of arteries clogging again.
You can prepare for emergencies: know your personal risk, carry a list of medicines, and teach family members signs of heart attack and stroke. If you have chest pain that lasts more than a few minutes or sudden neurological signs, don't wait - call emergency services.
If you want practical next steps, start with a primary care visit to get screening for blood pressure, cholesterol, and diabetes. Ask about testing for arterial blockages if you have leg pain or repeated chest discomfort. Small changes now reduce the odds of a big event later.
Follow-up care often includes cardiac rehab or stroke rehab with exercise plans, diet coaching, and medication checks. Your team may recommend an angiogram to map blockages or a carotid procedure to lower stroke risk. Ask about home blood pressure monitoring and how often to repeat tests. If you have questions about medicines, bring a list to every visit.
Don't ignore mild or strange symptoms. Early action saves tissue and improves recovery. Talk honestly with your doctor about risks and treatment options.