When you have a severe drug allergy, a simple piece of jewelry can save your life. It’s not just a fashion accessory-it’s your voice when you can’t speak. If you’ve ever had an anaphylactic reaction to penicillin, sulfa, morphine, or any other medication, wearing a medical alert bracelet isn’t optional. It’s essential. Emergency responders see hundreds of patients every shift. They don’t have time to guess what’s wrong. They look for the bracelet first.
Why a Medical Alert Bracelet Matters
Every year, over 1.5 million Americans visit the emergency room because of drug allergies. Many of these cases involve people who were given the wrong medication while unconscious, confused, or unable to communicate. A 2023 survey by American Medical ID found that 95% of emergency medical professionals check for medical alert jewelry right away. And 95% of them look at the wrist. That’s your bracelet. Not your phone. Not your wallet. Not your medical card tucked in your purse.
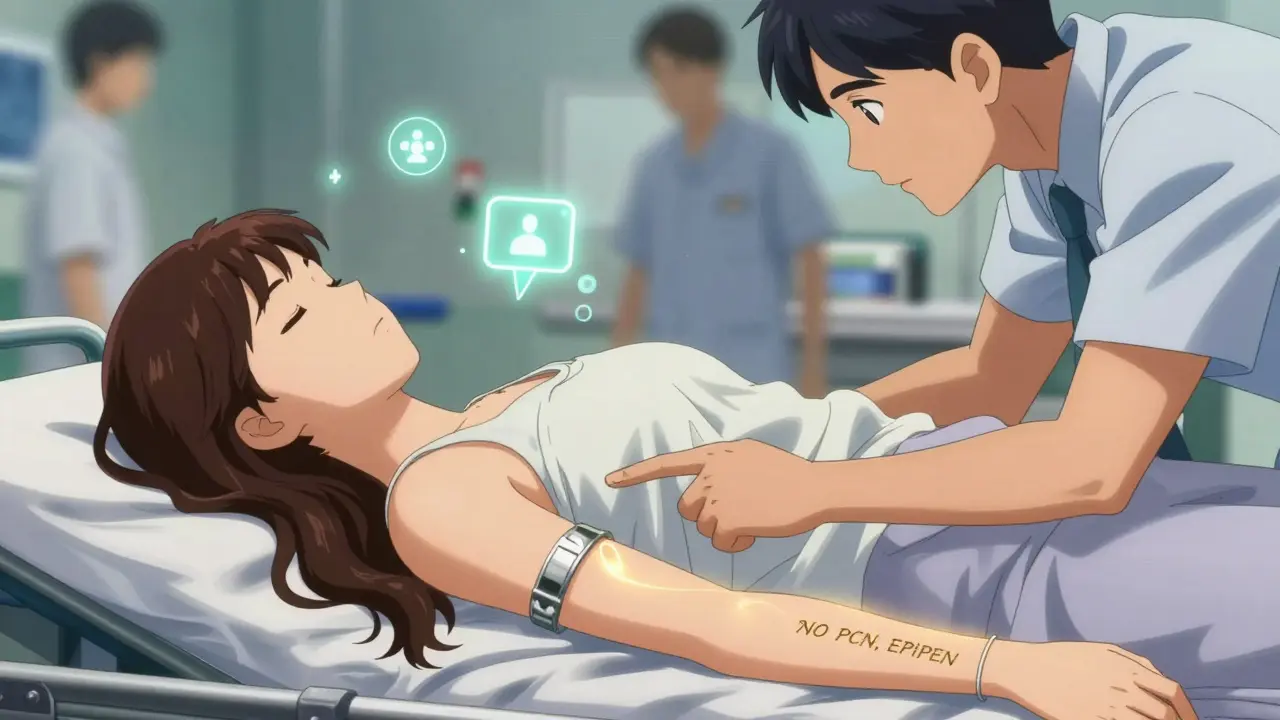
Think about it: You’re in a car crash. You’re unconscious. You’re rushed to the ER. The doctor is about to give you antibiotics for a suspected infection. If you’re allergic to penicillin and no one knows, you could go into cardiac arrest. But if you’re wearing a bracelet that says NO PCN, they stop. They check your chart. They call for an alternative. That’s the difference between a 10-minute delay and a life saved.
What to Engrave on Your Medical Alert Bracelet
Space is limited. You can’t fit your whole medical history. But you can fit the most critical info. Here’s what experts from the American College of Allergy, Asthma, and Immunology and MedicAlert Foundation recommend:
- Your name (optional but helpful)
- Primary drug allergy: NO PCN (penicillin), ALGYS: SULFA, ALGYS: MORPHINE
- Any other drug allergies (use abbreviations: ALGYS = allergies)
- Emergency medication: EPI PEN (if you carry an epinephrine auto-injector)
- Emergency contacts: ICE: MOM 555-123-4567 (In Case of Emergency)
- Any life-threatening conditions: DIABETIC, ASTHMA, NO GLUTEN (if celiac disease causes cross-reactions)
Avoid full sentences. Don’t write “I am allergic to penicillin.” Use NO PCN. Don’t write “I have an epinephrine auto-injector.” Use EPI PEN. These are the universal codes emergency staff are trained to recognize. Using non-standard terms like “allergic to amoxicillin” instead of “NO PCN” can cause confusion-amoxicillin is a type of penicillin. Standardization saves seconds. Seconds save lives.
Where to Wear It
Wear it on your dominant wrist. If you’re right-handed, wear it on your right wrist. That’s where most ER staff check first. Necklaces are also acceptable, but 68% of responders check the neck, while 95% check the wrist. The wrist wins.
Make sure it’s visible. Don’t tuck it under a long sleeve or cover it with a watch. If you wear a watch, put the medical ID on the other wrist. If you’re wearing a long-sleeved shirt, roll it up. Make it easy to see. Emergency teams don’t have time to search. They scan. They look. They act.
Wear it 24/7. Even when you’re sleeping. Even when you’re showering. Even when you’re at the gym. Allergic reactions don’t wait for convenient hours. A reaction can happen during a routine blood draw, a dental visit, or a routine surgery. You don’t get to pick the time.
What Material to Choose
Your bracelet needs to be durable and safe. It should be made of medical-grade materials that won’t cause a reaction themselves. Avoid nickel. Avoid cheap metals. Go for:
- Surgical stainless steel
- Titanium
- Medical-grade silicone
Silicone bands are lightweight and flexible. They’re great for active people. They’re also less likely to snag or break. Stainless steel is more traditional and feels more substantial. Both are hypoallergenic. Avoid plated jewelry-it can wear off and expose you to allergens like nickel.
Size matters too. Most bracelets are 6 to 8 inches long. They should fit snugly but not tight. You should be able to slide a finger underneath. Too loose, and it slips off. Too tight, and it cuts circulation.

Don’t Skip the Digital Backup
A bracelet is your first line of defense. But it’s not your only one. In 2024, MedicAlert Foundation and American Medical ID both launched digital profiles linked to QR codes on the back of their IDs. Scan the code with a smartphone, and first responders get your full medical history: allergies, medications, conditions, emergency contacts, even your doctor’s number.
This doesn’t replace the bracelet. It enhances it. If your engraving fades, or if you’re wearing a silicone band that’s hard to read in low light, the QR code gives responders a second chance. Some newer silicone bands even have NFC chips-you tap your phone to them, and the info pops up instantly.
Set up your digital profile with your current medications, allergies, and two emergency contacts. Update it every time your prescription changes. Outdated info is one of the top reasons medical alerts fail. A 2023 study found that 33% of cases with incorrect alerts were due to unupdated information.
Real Stories That Prove It Works
A 42-year-old woman in Oregon went to the ER with low blood sugar. She was confused, couldn’t speak clearly. The nurse started to give her a broad-spectrum antibiotic. But the bracelet said: ALGYS: CEPHALOSPORIN. The nurse paused. They ran a test. Turned out she had a severe allergy to that class of antibiotics. They gave her the right treatment. She went home the next day.
A man in Florida was unconscious after a seizure. He had a bracelet that said NO PCN, EPI PEN. The paramedic saw it, flagged the chart, and avoided giving him penicillin-based drugs. Later, he found out the ER had planned to give him ampicillin-a penicillin derivative. His bracelet stopped it.
On Reddit, a user named u/EpiPenSurvivor wrote: “I had my appendix out. I was under anesthesia. I had no idea what they were giving me. My bracelet said NO PCN, EPI PEN, ALGYS: SULFA. The surgeon asked the anesthesiologist, ‘Did you check his ID?’ They did. They switched the antibiotic. I woke up alive.”
Common Mistakes to Avoid
- Using non-standard abbreviations like “allergic to penicillin” instead of “NO PCN”
- Wearing it only on special occasions
- Letting the engraving fade or get scratched
- Not updating it after a new allergy is diagnosed
- Choosing a bracelet that’s too small to read
- Putting it on the wrong wrist
- Assuming your family or doctor will tell responders
One of the biggest mistakes? Thinking, “I’ll just tell them if I’m conscious.” But what if you’re not? What if you’re in a coma? What if you’re having a stroke? What if you’re a child? What if you’re elderly and confused? Your bracelet doesn’t forget. It doesn’t panic. It doesn’t get tired. It’s always there.
How to Get One
You can buy medical alert bracelets from trusted providers like MedicAlert Foundation, American Medical ID, or Lauren’s Hope. Most start at $25. Some insurance plans cover them if you have a documented history of anaphylaxis. Check with your doctor-they can write a letter of medical necessity.
When you order, make sure you can preview the engraving before it’s done. Read it out loud. Ask a friend to read it. Make sure it’s clear. Make sure the font is large enough. If you can’t read it from 12 inches away, it’s too small.
What If You Can’t Wear a Bracelet?
If you have a skin condition, nerve damage, or a job that doesn’t allow jewelry (like construction or food service), you can wear a medical alert necklace, anklet, or even a wallet card in a clear plastic sleeve. But these are less reliable. Necklaces can be hidden under shirts. Wallet cards can be lost. A bracelet stays on your wrist. It’s the gold standard.
Some people use medical alert apps on their phone. But if your phone is dead, broken, or locked, it’s useless. Physical jewelry works without batteries. It works during power outages. It works in the back of an ambulance. That’s why 87% of people with severe drug allergies still wear physical IDs-even in 2025.
Final Thought: It’s Not a Choice. It’s a Safety Net.
You don’t wear a seatbelt because you think you’ll crash. You wear it because you might. Same with a medical alert bracelet. You don’t wear it because you expect to have a reaction. You wear it because you might. And if you do, you want the people trying to save you to know exactly what to do-and what not to do.
Can I just rely on my phone’s health app instead of a bracelet?
No. Phone apps require power, internet, and a functioning screen. Emergency responders can’t wait for you to unlock your phone. They can’t scan a QR code if your phone is cracked or dead. A medical alert bracelet works without batteries, without Wi-Fi, and without a password. It’s the only reliable tool that works the moment you’re brought into the ER unconscious.
What if I’m allergic to the metal in the bracelet?
Choose a silicone band. Medical-grade silicone is hypoallergenic and designed for people with sensitive skin. Brands like Lauren’s Hope and American Medical ID offer silicone options with laser-engraved text that won’t fade. Avoid plated or nickel-containing metals. If you’re unsure, ask your allergist for a patch test before buying.
Do children need medical alert bracelets for drug allergies?
Yes. Children can’t always explain their allergies, especially during a reaction. Many parents choose silicone bands with fun designs for kids. The same rules apply: list the allergy clearly (e.g., “NO AMOXICILLIN”), include ICE contacts, and wear it 24/7. Schools and daycare centers should be informed, but the bracelet is the only thing that travels with them.
How often should I replace my medical alert bracelet?
Replace it if the engraving becomes unreadable, the band cracks, or you get a new allergy. Most metal bracelets last 5-10 years. Silicone bands last 1-3 years, depending on wear. Check your bracelet every 6 months. If you can’t read the text clearly, replace it. Your life depends on it.
Will insurance cover the cost of a medical alert bracelet?
Some do. If you’ve had a documented anaphylactic reaction, your doctor can write a letter stating the bracelet is medically necessary. Submit it to your insurance with a CPT code for durable medical equipment. Many Medicare Advantage and private plans cover it. If not, most bracelets cost under $40-less than a monthly coffee habit.
If you have a severe drug allergy, don’t wait for a close call to act. Get your bracelet. Wear it. Update it. Make sure your emergency contacts know about it. This isn’t about being cautious. It’s about being prepared. Your life depends on it.