Combining kava with sedative medications isn’t just a bad idea-it can land you in the hospital. If you’re taking anything that makes you drowsy-like Xanax, Valium, lorazepam, or even sleep aids-and you’re also using kava for anxiety or relaxation, you’re playing with fire. The risks aren’t theoretical. People have ended up with liver failure, extreme drowsiness, and even needed liver transplants after mixing the two.
What Exactly Is Kava?
Kava comes from the roots of the Piper methysticum plant, traditionally used in Pacific Island ceremonies for its calming effects. In the U.S., it’s sold as a dietary supplement in capsules, teas, or liquid extracts. Its active compounds, called kavalactones, work on the brain to reduce anxiety and promote muscle relaxation. A typical dose ranges from 70 to 250 mg of kavalactones per day. But here’s the catch: not all kava is the same. Traditional water-based preparations from noble kava varieties are much safer than alcohol-based extracts sold in bottles at health stores. Those extracts can contain up to 300 mg of kavalactones per serving-far more than what’s been safely studied.
Why Kava and Sedatives Are a Dangerous Mix
Sedative medications-benzodiazepines, barbiturates, sleep pills, even some antidepressants-slow down your central nervous system. Kava does the same thing. When you combine them, the effect isn’t just added-it’s multiplied. Studies show kava can increase the blood levels of drugs like midazolam by 27% because it blocks the liver enzymes (CYP3A4, CYP2D6, CYP2C9) that break them down. This means the medication stays in your body longer and stronger than intended.
Real-world cases back this up. In Sacramento County, a 42-year-old man took 300 mg of kava daily along with 2 mg of alprazolam. Within three months, his liver enzymes spiked to 2,840 U/L (normal is under 40). He developed jaundice and needed hospital care. Another patient, taking kava with diazepam, had a dangerous blood clotting issue with an INR of 4.2-far above the safe range. Both cases were directly linked to the combination.
Users on Reddit and Erowid report similar stories: being unable to stand for hours, slurred speech, confusion, and falling asleep mid-conversation. One person wrote: “I took kava with my 0.5 mg lorazepam and couldn’t get up for 8 hours.” That’s not relaxation-that’s overdose.
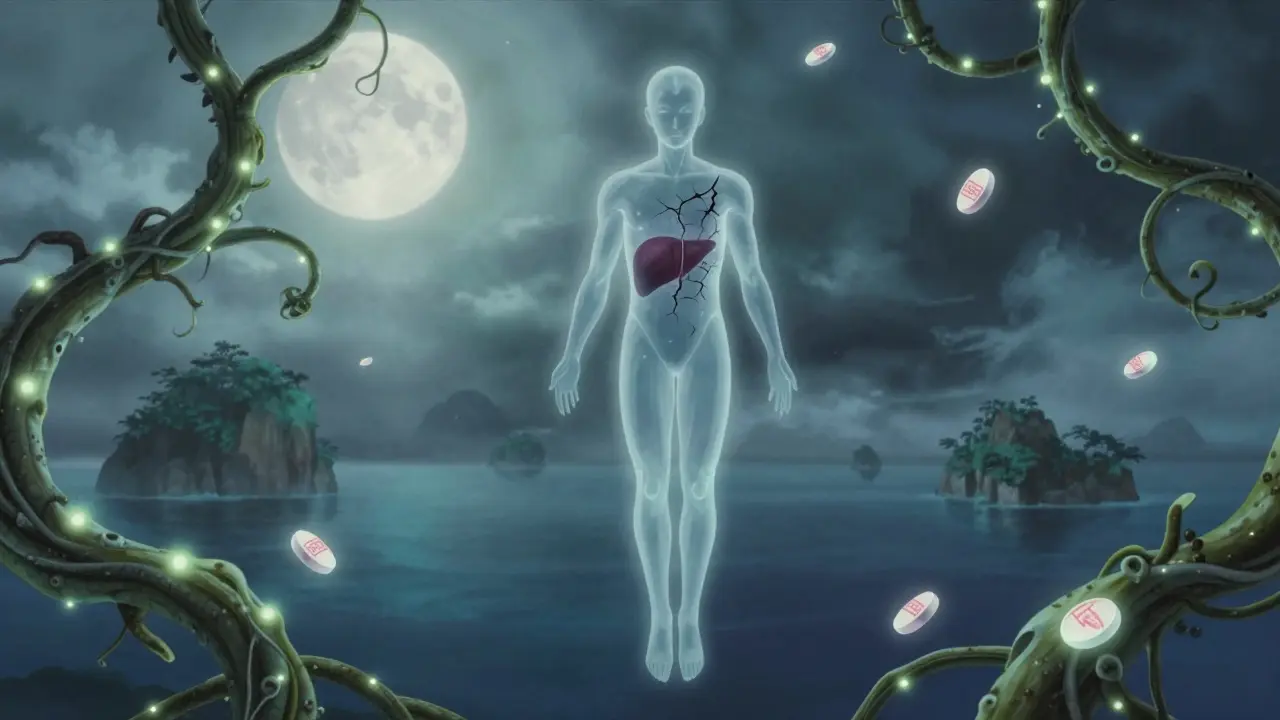
The Liver Risk Is Real-And Often Hidden
The FDA issued a warning about kava and liver damage back in 2002. Since then, over 25 international cases have been reported, including several liver transplants. The problem? Liver damage from kava doesn’t come with obvious warning signs until it’s too late. Fatigue, nausea, dark urine, yellowing of the eyes or skin-these are late symptoms. By then, significant damage may already be done.
What’s worse, most people don’t tell their doctors they’re using kava. Sacramento County researchers found only 22% of patients with liver problems mentioned kava use when asked. Doctors don’t always think to ask. Pharmacists rarely screen for it. And because kava is sold as a supplement, there’s no requirement for safety labeling or dosage warnings on the bottle.
Even if you’re not on sedatives, kava can still hurt your liver-especially if you take more than 250 mg daily, use it for longer than three months, or use alcohol-based extracts. The European Food Safety Authority says there’s no safe level for people on medications that affect the same liver enzymes. Australia’s health agency says the risk is low but real, especially with long-term, high-dose use.

How Kava Compares to Other Herbal Sleep Aids
Not all herbal supplements are risky like kava. Valerian root, for example, has very few documented drug interactions. Chamomile and lemon balm are generally safe with sedatives, though they can add mild drowsiness. Kava is in a different league. It doesn’t just make you sleepy-it interferes with how your body processes medications. That’s why it’s rated as a “major” interaction by WebMD, while most other herbs are “mild” or “moderate.”
Prescription anxiety meds like buspirone or SSRIs have predictable dosing and are monitored for liver safety. Kava doesn’t. One bottle might have 100 mg of kavalactones; the next might have 280 mg. There’s no standardization. And if you’re buying online-which most people do-you have no idea what’s actually in it.
Who Should Avoid Kava Completely?
Here’s who needs to say no:
- Anyone taking sedatives, sleep aids, anti-anxiety meds, or alcohol
- People with existing liver disease, hepatitis, or elevated liver enzymes
- Those on medications metabolized by CYP2D6, CYP2C9, or CYP3A4-this includes statins, blood thinners, some antidepressants, and even certain painkillers
- Anyone using kava for more than three months
- People using alcohol-based extracts, powders, or concentrated tinctures
If you have a history of alcohol abuse, depression, or liver issues, kava is not worth the risk-even without other medications.
What If You’re Already Using Kava With Sedatives?
Don’t stop your prescription meds cold turkey. But do talk to your doctor or pharmacist immediately. They can help you safely taper off one or both if needed.
Here’s what to do right now:
- Stop taking kava if you’re on any sedative medication.
- Get a liver function test (ALT, AST, bilirubin) if you’ve used kava for more than a month.
- If your ALT is more than three times the upper limit of normal, stop kava immediately. Most mild cases recover within two months after stopping.
- Switch to non-interacting alternatives like mindfulness, therapy, or FDA-approved medications if anxiety is the goal.
- Tell every healthcare provider you see that you’ve used kava-even if you stopped months ago.
There’s no safe way to combine them. The CDC recommends that people on sedatives limit kava to 70 mg daily with biweekly liver tests-but even that’s not advised. The safest choice is to avoid kava entirely if you’re on any CNS depressant.

Why Is Kava Still Sold in the U.S.?
The U.S. is one of the only developed countries where kava is still widely available. The FDA has issued warnings since 2002, but because it’s classified as a dietary supplement under the 1994 DSHEA law, it doesn’t need pre-market approval. The industry argues that traditional water-based kava is safe, and that most liver cases involved poor-quality extracts or other factors. But the evidence doesn’t support that claim. The World Health Organization found that traditional preparations have 9 times fewer adverse events than commercial extracts.
Still, 41% of naturopathic doctors in the U.S. recommend kava for anxiety, while only 3% of board-certified psychiatrists do. That gap is dangerous. Patients trust their naturopaths-but those providers often lack training in drug interactions or liver toxicity.
States are starting to act. California issued warnings in 2024. New York is pushing for mandatory liver toxicity labels. But until federal rules change, the burden is on you to know the risks.
What Are the Safer Alternatives?
If you’re using kava for anxiety or sleep, here are better options:
- Cognitive Behavioral Therapy (CBT): Proven to work as well as medication for anxiety, with no side effects.
- Mindfulness and breathing exercises: Studies show they reduce anxiety within weeks.
- Prescription alternatives: Buspirone, SSRIs, or low-dose trazodone (for sleep) are safer and regulated.
- Non-interacting herbs: Chamomile tea, lemon balm, or passionflower (in moderation) are low-risk for most people.
None of these will give you the same immediate “high” as kava-but they won’t shut down your liver either.
Final Takeaway
Kava isn’t a harmless herbal remedy. When mixed with sedatives, it’s a ticking time bomb for your liver and your brain. The risks aren’t rare. They’re documented, preventable, and often ignored. If you’re taking any medication that makes you drowsy, don’t risk it. The few minutes of calm you get from kava aren’t worth months of recovery-or a liver transplant.
Stop. Talk to your doctor. Get tested. Choose safer paths. Your liver will thank you.