When you start a new medication, your doctor might say, "You could experience some side effects." But what does that really mean? And if you feel sick after taking it, is it a side effect-or something more serious? The truth is, most people use these terms interchangeably, but in medicine, they’re not the same. Confusing them can lead to unnecessary fear, wrong decisions, and even dangerous outcomes. Understanding the difference between side effects and adverse drug reactions isn’t just academic-it’s life-saving.
What Exactly Is a Side Effect?
A side effect is a predictable, dose-related reaction that happens because of how a drug works in your body. It’s not a mistake. It’s not an accident. It’s built into the drug’s design. For example, antihistamines make you drowsy because they cross into your brain and block histamine, which helps keep you awake. That drowsiness? That’s a side effect. It’s expected. It’s documented. And it shows up in clinical trials far more often in people taking the drug than in those taking a placebo. Side effects are usually mild and manageable. Think dry mouth from antidepressants, nausea from antibiotics, or dizziness from blood pressure meds. They’re listed in the patient information leaflet because they’re common enough to matter. About 80-85% of all drug-related problems fall into this category. These are the Type A adverse reactions-predictable, tied to dosage, and often avoidable by adjusting the dose or timing. Here’s the key: a side effect only counts as one if studies prove it’s caused by the drug. In a 2020 JAMA study on the blood thinner apixaban, headaches occurred in 12.3% of people taking the drug and 11.8% taking a sugar pill. That tiny difference? It means headache isn’t a side effect-it’s just something that happens sometimes, whether you’re on the drug or not.What Counts as an Adverse Drug Reaction?
An adverse drug reaction (ADR) is any harmful, unintended response to a medication taken at normal doses. But here’s the catch-not all ADRs are side effects. ADRs include side effects, but they also include rare, unpredictable reactions that have nothing to do with the drug’s main action. These are the Type B reactions-unpredictable, not dose-related, and often immune-driven. For example, a severe skin rash from penicillin isn’t because penicillin is supposed to cause rashes. It’s because your immune system overreacts to it. That’s an ADR, but not a side effect. Another example: liver damage from acetaminophen at normal doses in someone with a rare genetic variation. That’s an ADR, too. The World Health Organization has defined ADRs since 1972, and the FDA still uses the term in official guidance. But here’s where things get messy: the FDA sometimes uses "side effect" and "adverse reaction" as synonyms. That’s where confusion starts. In research and clinical practice, though, they’re kept separate for a reason.Adverse Events: The Big Umbrella
Now let’s bring in adverse events. This is the broadest category. An adverse event is simply any negative health occurrence that happens after you take a drug-no matter if the drug caused it or not. Imagine you start a new cholesterol drug and three days later, you fall and break your hip. The fall wasn’t caused by the drug. But because it happened after you started taking it, it’s recorded as an adverse event. Same thing if you get the flu while on a diabetes medication. Or if you have a panic attack. Or if your arthritis flares up. None of these are caused by the drug-but they’re still logged. In clinical trials, researchers record every single adverse event. Then they compare rates between the drug group and the placebo group. Only if the rate is significantly higher in the drug group does it become a side effect. Everything else? Just an adverse event. That’s why millions of adverse event reports get filed every year with the FDA-but only about a third turn out to be true adverse drug reactions.
Why the Difference Matters in Real Life
This isn’t just semantics. Mixing up these terms leads to real harm. A 2021 study found that 43% of patients stopped taking life-saving medications because they thought every bad feeling was a "side effect." One man quit his blood thinner after getting a headache. Another stopped her antidepressant because she felt tired. Neither headache nor fatigue was actually caused by the drug. But because they were labeled "side effects" in conversations with doctors, patients assumed they had no choice but to stop. Doctors make the same mistake. A 2021 survey by the Institute for Safe Medication Practices showed 68% of healthcare workers use "side effect" and "adverse reaction" interchangeably in charts. That leads to inaccurate reporting, flawed safety data, and even insurance denials. One 2023 study found that 12% of medication-related insurance claims were denied because the doctor wrote "side effect" when they meant "adverse event"-and insurers don’t pay for problems that aren’t drug-caused.How Doctors Tell the Difference
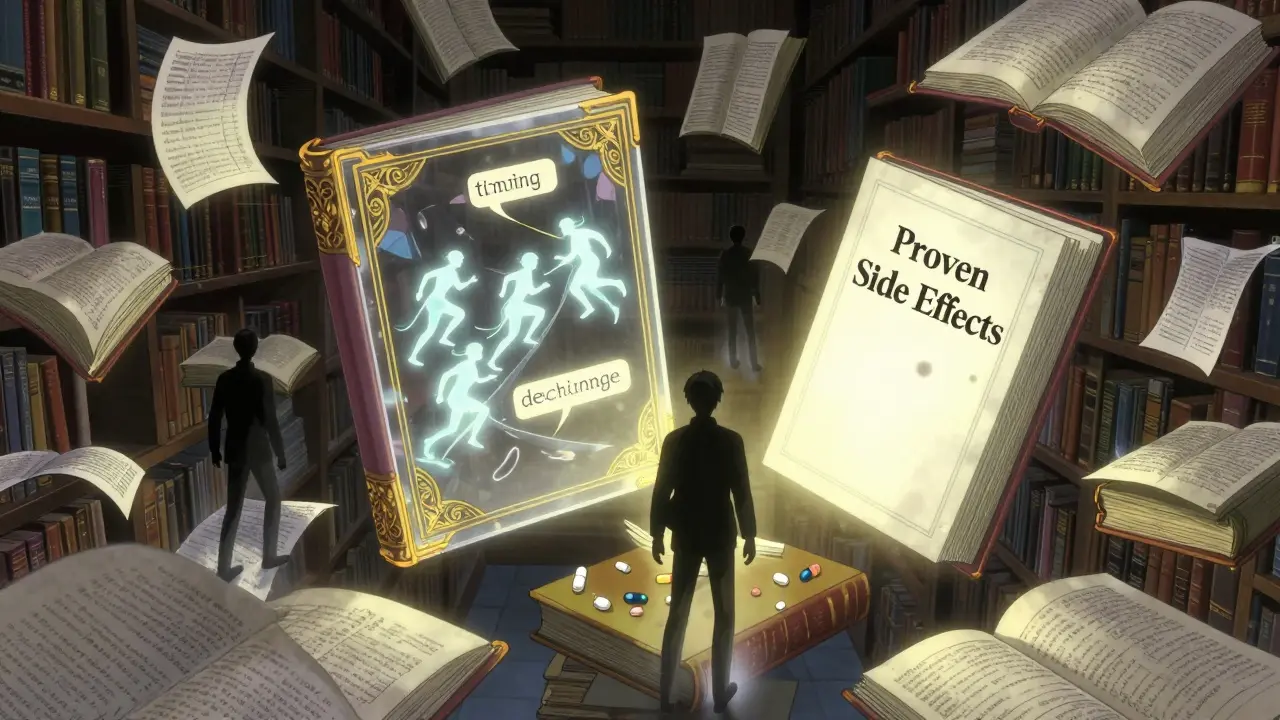
It’s not guesswork. There’s a method. At top hospitals like UCSF, doctors use a 3-step process:- Timing: Did the symptom start after the drug was introduced? If yes, it’s suspicious.
- Dechallenge: If you stop the drug and the symptom goes away, that’s a clue.
- Rechallenge: If you restart the drug and the symptom comes back-strong evidence it’s caused by the drug.
What You Should Do as a Patient
You don’t need to be a doctor-but you can ask smarter questions:- "Is this a common side effect, or could it be something else?"
- "Has this been proven to be caused by the drug, or is it just something that happened around the same time?"
- "If I stop this, will it go away?"
The Future: Better Tools, Fewer Mistakes
Technology is helping. New AI tools from companies like ArisGlobal can now scan patient records and flag potential side effects with 41% more accuracy than before. The FDA’s new Modernization Act 2.0 requires these systems to clearly distinguish between adverse events and true reactions by 2025. The WHO’s drug dictionary now lists over 14,000 confirmed side effects-up from under 12,000 just three years ago. And pharmacogenomic testing is starting to tell us who’s genetically at risk for certain reactions. For example, people with a certain gene variant are nearly nine times more likely to have dangerous bleeding on the blood thinner clopidogrel. That’s not a side effect for everyone-it’s a side effect for them. The goal? To stop treating every bad feeling as a drug problem. To stop scaring people into stopping their meds. To make sure only the real dangers get labeled as side effects.Final Takeaway
Side effects are predictable, common, and tied to how the drug works. Adverse drug reactions include side effects-but also rare, unpredictable dangers. Adverse events are anything bad that happens after you take a pill, whether the pill caused it or not. Knowing the difference helps you make better decisions. It helps your doctor treat you better. And it helps keep the whole system of drug safety working the way it should.Next time you hear "side effect," don’t panic. Ask: "Is this expected? Is it proven? Or is it just a coincidence?" That’s the real power of understanding the difference.