Heat Tolerance Risk Calculator
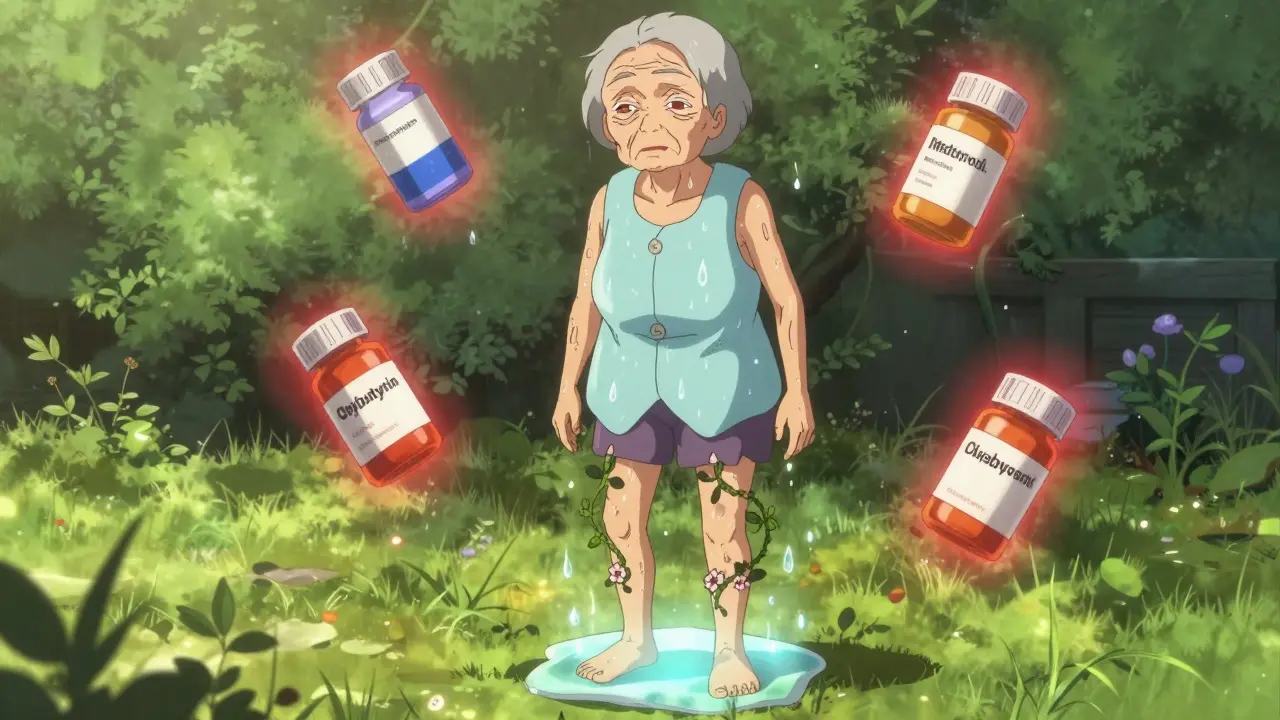
Medication Risk Assessment
This tool helps you understand your risk of heat intolerance based on medications you take and other factors. Note: This is not medical advice.
Risk Assessment Results
When the temperature climbs, most people sweat to cool down. But if you’re taking certain medications, your body might not be able to do that - and that can be dangerous. Heat intolerance isn’t just about feeling hot. It’s when your body can’t regulate its temperature properly, leading to cramps, dizziness, confusion, or even life-threatening heat stroke. The problem? Decreased sweating from common prescriptions is more widespread than most people realize.
Why Some Medications Stop You from Sweating
Sweating is your body’s main way to release heat. When your core temperature rises, nerves signal sweat glands to release fluid onto your skin. As it evaporates, it cools you down. But certain drugs interfere with this process - sometimes in ways you wouldn’t expect. Anticholinergic medications are among the worst offenders. These include drugs like oxybutynin (for overactive bladder), diphenhydramine (Benadryl), and some tricyclic antidepressants. They block acetylcholine, a chemical your body needs to activate sweat glands. Studies show these drugs can cut sweating by 60-80%. That means even on a mild 27°C (80°F) day, your body can’t cool itself effectively. Diuretics like hydrochlorothiazide and chlorthalidone work by flushing out extra fluid. That’s great for lowering blood pressure, but it also means less water available for sweat. Research from Santa Monica Family Physicians shows these drugs can reduce sweat production by 30-50%. You might not even feel thirsty, but your body is running on empty. Beta blockers - such as metoprolol and propranolol - don’t stop sweating directly. Instead, they limit blood flow to your skin. Normally, when you’re hot, blood vessels widen to carry heat to the surface. Beta blockers prevent that. One study found they reduce skin blood flow by 25-40%, trapping heat inside your body. Even newer weight-loss drugs like semaglutide (Ozempic, Wegovy) are linked to heat problems. They suppress thirst signals by 40-50%, so you drink less even when you should. Combine that with reduced sweating, and dehydration hits fast.High-Risk Medication Classes
Not all medications affect heat the same way. Some are riskier than others. Here are the top five classes with the strongest links to heat intolerance:- Anticholinergics: Oxybutynin, tolterodine, diphenhydramine, scopolamine. Reduce sweating by 60-80%.
- Diuretics: Hydrochlorothiazide, chlorthalidone. Cause fluid loss of 1.5-2.5 liters daily, cutting sweat capacity.
- Beta blockers: Metoprolol, propranolol. Cut skin blood flow by 25-40%, preventing heat release.
- Antipsychotics: Olanzapine, risperidone, haloperidol. Disrupt both sweating and brain temperature control. Risk of heat stroke even at 27-32°C (80-90°F).
- Stimulants: Methylphenidate, amphetamines. Increase internal heat by 15-25% while blocking cooling mechanisms.
Tricyclic antidepressants like amitriptyline are especially risky - they reduce sweating by 65-75%. In contrast, newer SSRIs like fluoxetine may actually increase sweating, which can lead to dehydration instead. The type of medication matters just as much as the condition it treats.
Who’s Most at Risk?
It’s not just about the drug. It’s about who’s taking it. Older adults are especially vulnerable. As we age, our sweat glands naturally become less active. Add in multiple medications, and the risk skyrockets. The American Geriatrics Society says people over 65 taking five or more medications have a 300% higher chance of heat stroke than younger, healthier people. People taking three or more heat-affecting drugs at once are also at extreme risk. A 2022 CDC report found that 18-22% of all heat-related ER visits among adults over 50 were tied to medication combinations. Lithium, used for bipolar disorder, is particularly dangerous. Dehydration can spike lithium levels by 25-35%, leading to toxicity - even at temperatures as low as 29°C (85°F). Climate change is making this worse. With 2023 being the hottest year on record, and heat waves becoming more frequent and intense, the number of medication-related heat illnesses is climbing. Between 2010 and 2022, hospitalizations for heat illness among people on these drugs rose by 67%.Warning Signs You Can’t Ignore
You don’t have to wait for heat stroke to realize something’s wrong. Early signs often show up within 30-90 minutes of being in the heat:- Cramps in arms, legs, or stomach (65% of cases)
- Dizziness or lightheadedness (55%)
- Headache (70%)
- Flushed, dry, or hot skin (45%)
- Nausea or vomiting (35%)
- Weakness or fatigue (60%)
- Lack of sweating - or sweating that suddenly stops (85% of cases)
If you notice any of these - especially if you’re on one of the high-risk meds - get out of the heat immediately. Don’t wait for confusion, rapid heartbeat, or loss of consciousness. Those are signs of heat stroke, which can be fatal.
How to Stay Safe in the Heat
If you’re on medication that affects sweating, you need a plan. Here’s what works:- Drink more water: Add 500-1000 mL (17-34 oz) to your daily intake during hot weather. Don’t wait until you’re thirsty - especially if you’re on GLP-1 drugs.
- Avoid the sun between 10 AM and 4 PM: That’s when UV exposure and heat are strongest. Plan outdoor tasks for early morning or evening.
- Use air conditioning: If you don’t have it at home, go to a library, mall, or cooling center. Even a few hours of relief helps.
- Check your weight daily: A drop of 2% or more in body weight means you’re dehydrated. Weigh yourself in the morning before eating or drinking.
- Wear cooling gear: For those on antipsychotics or anticholinergics, cooling vests can lower core temperature by 0.5-1.0°C - enough to prevent heat stroke.
- Use SPF 30+ sunscreen: Some blood pressure meds like calcium channel blockers make your skin more sensitive to sunburn.
Don’t stop your meds without talking to your doctor. But do ask: “Could this medication affect how I handle heat?” If you’re on multiple drugs, ask for a heat risk review. Some clinics now use electronic health records that flag high-risk combinations during summer months.
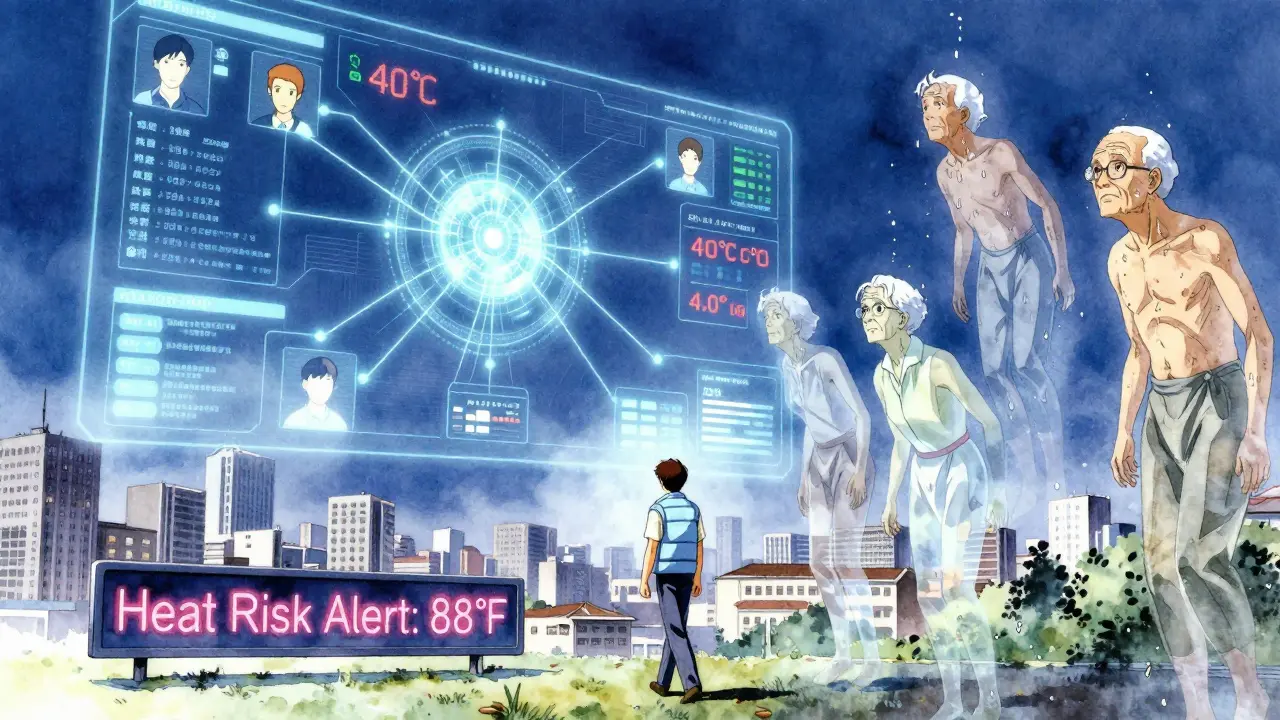
New Tools to Help You Stay Cool
Technology is catching up. In December 2023, the FDA approved TempTraq - the first wearable device that continuously monitors core body temperature. It’s designed specifically for people on heat-affecting medications. It sends alerts if your temperature rises too high, even before you feel symptoms. The NIH is also funding a $2.5 million study starting in September 2024 to build AI tools that predict individual heat risk based on medication lists, age, and climate data. This could one day tell you: “Your combo of metoprolol and hydrochlorothiazide puts you at high risk when it’s over 88°F.”When to Call for Help
Heat stroke is a medical emergency. Call 911 if someone:- Has a body temperature above 40°C (104°F)
- Is confused, agitated, or unconscious
- Has no sweat despite being hot
- Has a rapid pulse or shallow breathing
While waiting for help, move the person to a cool place, remove excess clothing, and apply cold packs to the neck, armpits, and groin. Don’t give them fluids if they’re confused - they could choke.
Can I still exercise if I’m on medication that causes decreased sweating?
Yes - but you need to adjust. Avoid outdoor workouts during peak heat (10 AM-4 PM). Stick to indoor, air-conditioned spaces. Reduce intensity and take longer breaks. Monitor your body closely: if you feel dizzy, stop immediately. Consider using a wearable temperature monitor like TempTraq if you’re on high-risk meds. Always hydrate before, during, and after.
Do over-the-counter drugs like Benadryl really cause heat intolerance?
Yes. Diphenhydramine (Benadryl) is an anticholinergic, and it blocks sweat gland activity. Even one dose can reduce sweating by 30-50%. Many people don’t realize it’s in allergy, cold, and sleep aids. If you’re taking it regularly - even just at night - you’re at higher risk during hot weather. Look for “anticholinergic” on the label or ask your pharmacist.
Is heat intolerance permanent if I take these medications long-term?
No - the effect is reversible. Once you stop the medication (under medical supervision), your body’s ability to sweat usually returns within days to weeks. But while you’re on it, the risk stays. That’s why prevention matters more than waiting for side effects to fade. Never quit meds abruptly - talk to your doctor about alternatives if heat is a major concern.
Why do some blood pressure meds make me more sensitive to the sun?
Some blood pressure drugs - especially calcium channel blockers, ACE inhibitors, and ARBs - can cause photosensitivity. This means your skin burns more easily and may react badly to UV light. It’s not the same as heat intolerance, but it adds to the risk. Always use SPF 30+ sunscreen, wear wide-brimmed hats, and avoid direct sun during peak hours.
Should I get my lithium levels checked during heat waves?
Yes - absolutely. Dehydration from heat and diuretics can cause lithium levels to spike by 25-35%, leading to toxicity. Symptoms include tremors, confusion, nausea, and kidney issues. The CDC recommends checking lithium levels before and after heat waves, especially if you’re sweating less or drinking less. Talk to your doctor about scheduling a blood test if temperatures are expected to stay above 29°C (85°F) for more than two days.
If you’re on any of these medications, don’t assume heat intolerance won’t happen to you. It’s silent, slow, and dangerous. The best defense is knowing your risks - and acting before it’s too late.