Simvastatin Interaction Checker
Check if your medications interact dangerously with simvastatin. This tool helps identify potentially life-threatening combinations with antibiotics, heart medications, grapefruit juice, and more.
Every year, millions of Americans take simvastatin to lower their cholesterol. It works. It’s cheap. And for many, it’s life-saving. But here’s the part no one talks about until it’s too late: simvastatin can kill you if you mix it with the wrong drugs-or even the wrong breakfast.
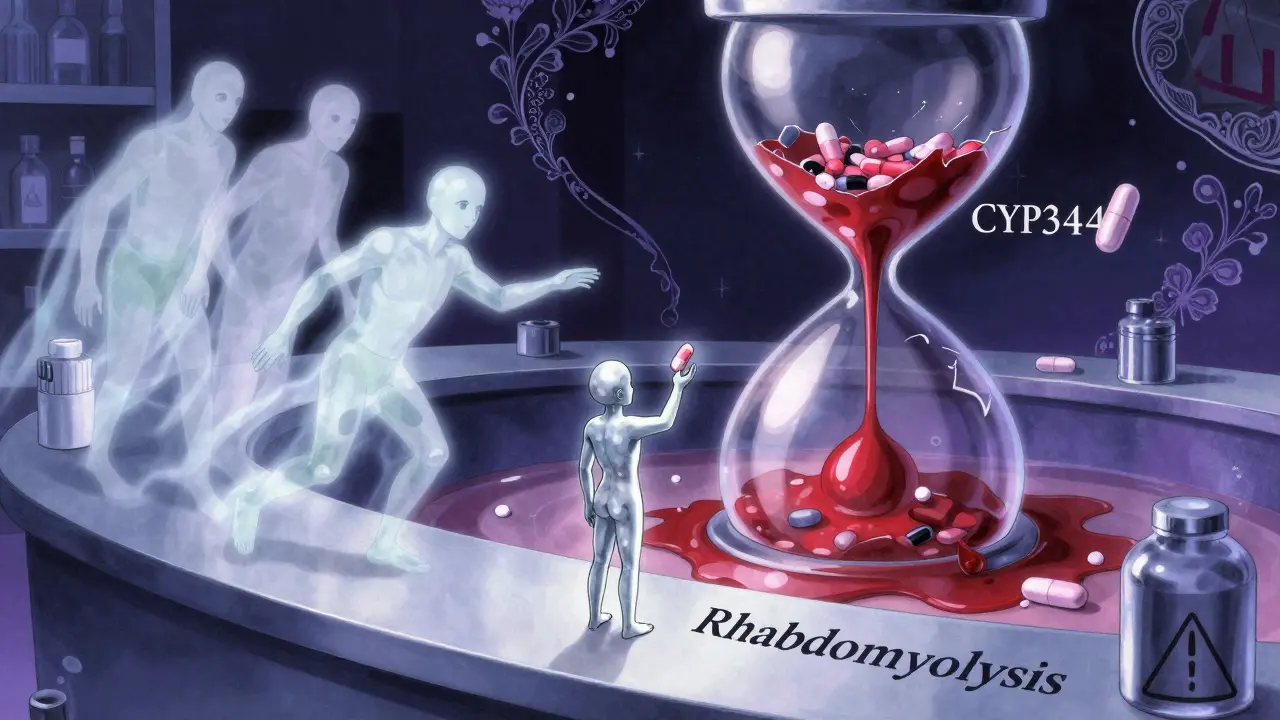
Let’s be clear: this isn’t about mild side effects. This is about rhabdomyolysis-a condition where your muscles start breaking down, flooding your bloodstream with toxic proteins that can shut down your kidneys and lead to death. The FDA has issued multiple warnings. Doctors have seen patients collapse within days. And yet, people still take simvastatin 80 mg with antibiotics, heart meds, or grapefruit juice-without realizing they’re playing Russian roulette with their muscles.
Why the 80 mg Dose Is a Red Flag
The 80 mg dose of simvastatin was once considered the gold standard for aggressive cholesterol control. But in 2011, the FDA pulled the plug on new prescriptions of this dose-not because it didn’t work, but because it was too dangerous.
Here’s the data: at 20-40 mg, the risk of muscle damage (myopathy) is about 0.08%. At 80 mg? It jumps to 0.61%. That’s nearly eight times higher. The SEARCH trial and FDA’s own adverse event database showed that people on 80 mg were far more likely to end up in the hospital with muscle pain, weakness, and dark urine-classic signs of rhabdomyolysis. By 2018, new prescriptions of the 80 mg dose had dropped by 82%. Today, less than 2% of new patients are started on it. Why? Because the risk doesn’t justify the benefit.
Even if you’ve been on 80 mg for years, that doesn’t mean it’s safe. Your body changes. You might start a new medication. Or you might forget you’re drinking grapefruit juice every morning. That’s when things go wrong.
The CYP3A4 Killer: How Drugs Turn Simvastatin Toxic
Simvastatin doesn’t just float around your body. It gets processed by a liver enzyme called CYP3A4. Think of this enzyme as a garbage disposal. When it’s working normally, it breaks down simvastatin so your body can get rid of it.
But if you take a drug that blocks CYP3A4, that disposal gets jammed. Simvastatin builds up in your blood-sometimes to levels 200-300% higher than normal. That’s when muscle damage starts.
Here are the real-world killers:
- Antibiotics: Clarithromycin and erythromycin. These are common for sinus infections and bronchitis. One prescription, and your simvastatin turns into a time bomb.
- Fungus fighters: Ketoconazole, itraconazole, voriconazole. Used for stubborn yeast or fungal infections. Avoid them completely if you’re on simvastatin.
- HIV drugs: Ritonavir, atazanavir, darunavir. These are strong CYP3A4 blockers. Even a single dose can be dangerous.
- Heart meds: Cyclosporine (for transplants), amiodarone, diltiazem, verapamil. These are often taken long-term, making the risk cumulative.
- Antidepressants: Nefazodone. Rarely prescribed now, but still out there.
The FDA says: if you absolutely must take one of these, your simvastatin dose must drop to 10 mg-or less. For some, like cyclosporine, you shouldn’t take simvastatin at all. Switch to pravastatin or rosuvastatin instead. They don’t rely on CYP3A4. They’re safer.
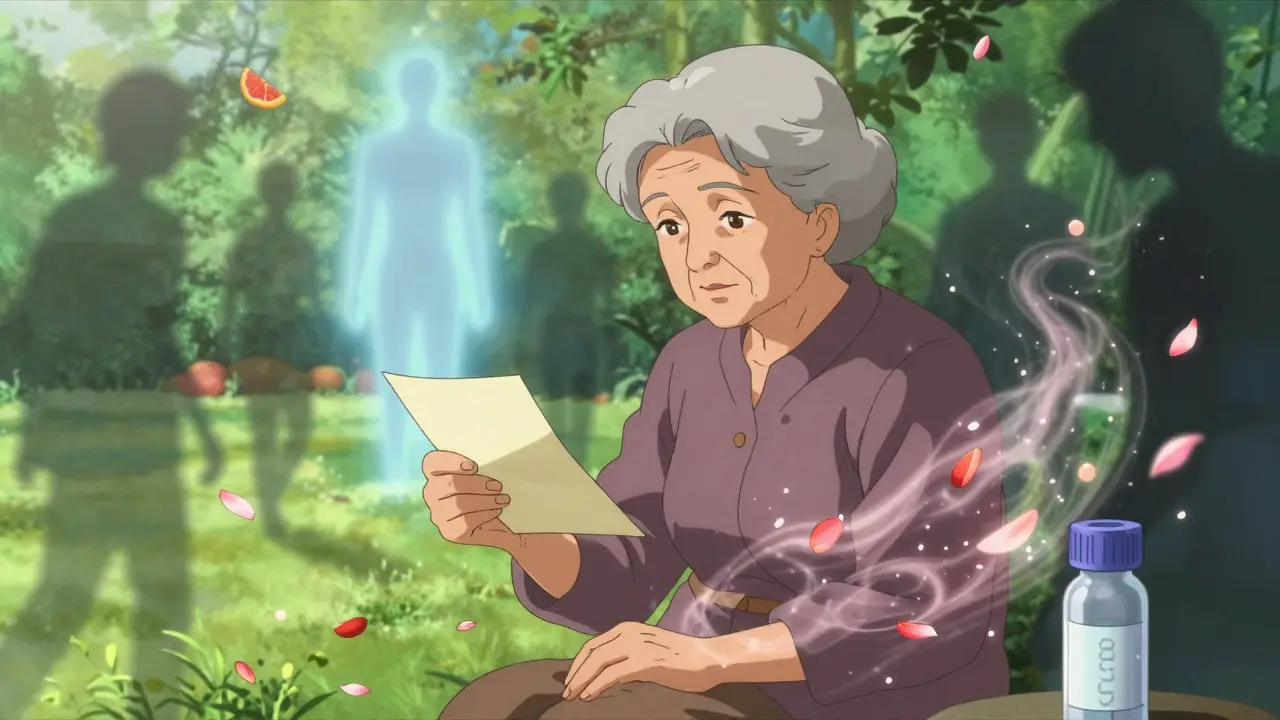
Grapefruit Juice: The Silent Killer in Your Refrigerator
You’ve probably heard you shouldn’t drink grapefruit juice with statins. But most people think it’s just a myth. It’s not.
A single 8-ounce glass of grapefruit juice can increase simvastatin levels in your blood by up to 260%. That’s not a little bump. That’s enough to push you into danger territory-even if you’re on 20 mg.
Studies show 43% of people on high-dose simvastatin still drink grapefruit juice regularly. They don’t realize it’s in smoothies, marmalade, or even flavored water. One pharmacist in Portland told me about a 68-year-old man who came in with severe muscle pain after drinking grapefruit juice every morning for years. He thought it was "healthy." He ended up in the hospital with rhabdomyolysis.
There’s no safe amount. No "just a little." If you’re on simvastatin, eliminate grapefruit and its juice completely. Or switch to an alternative statin.
Other Dangerous Mixes You Might Not Know About
It’s not just antibiotics and grapefruit. Other common drugs can also cause trouble:
- Colchicine: Used for gout. When taken with simvastatin, it increases muscle damage risk. This combo is especially dangerous in older adults and those with kidney problems.
- Fenofibrate or niacin: These are often added to statins to lower triglycerides. But together with simvastatin, they raise the risk of muscle injury. Many doctors now avoid this combo entirely.
- High-dose niacin: Even if you’re taking it as a supplement, it can interact. Don’t assume "natural" means safe.
And here’s the kicker: some of these interactions don’t show up until weeks later. You might feel fine for 10 days. Then, suddenly, your muscles ache. You can’t climb stairs. Your urine turns dark. By then, it’s often too late.
What You Should Do Right Now
If you’re on simvastatin, here’s your action plan:
- Check your dose. Are you on 80 mg? If yes, talk to your doctor immediately. Most people don’t need this dose anymore.
- Review every medication. Not just prescriptions-supplements, OTC painkillers, antibiotics you took last winter. Write them all down.
- Stop grapefruit. No exceptions. Not even once a week.
- Ask about genetic testing. The SLCO1B1 gene variant makes some people 4.5 times more likely to get muscle damage on simvastatin. Testing is cheap, fast, and can save your life.
- Get liver and muscle tests. Your doctor should check ALT, AST, and CK levels every 3-6 months. If you’re on a high dose or multiple interacting drugs, every 3 months is standard.
And if you’re a caregiver for an elderly parent? Watch for muscle weakness, fatigue, or dark urine. They might not tell you they’re hurting.
What Are the Alternatives?
You don’t have to stay on simvastatin. There are safer statins:
- Pravastatin: Not metabolized by CYP3A4. Safe with most other drugs.
- Rosuvastatin: Strong cholesterol-lowering power, fewer interactions.
- Pitavastatin: Newer, low interaction risk, effective even at low doses.
These aren’t more expensive. Generic pravastatin costs about $5 a month. Rosuvastatin is $10-$15. That’s less than your coffee habit. And you’re trading risk for safety.
Pharmacists can help you switch. Ask them to run a drug interaction check. Most pharmacies now have systems that flag dangerous combos before you even leave the counter.
Why This Still Happens
Doctors don’t always know every interaction. Patients forget to mention they took an antibiotic last month. Pharmacists are overloaded. And grapefruit juice? It’s marketed as a "superfood." People think it’s healthy. It’s not when you’re on simvastatin.
The truth? This isn’t about bad medicine. It’s about bad communication. You need to be your own advocate. If you’re on simvastatin, assume every new drug or supplement is a potential threat until proven safe.
And if you’ve been on simvastatin 80 mg for years? Don’t wait for symptoms. Talk to your doctor now. Switch. Test. Survive.
Can I take simvastatin with antibiotics?
No-not if they’re clarithromycin, erythromycin, or other strong CYP3A4 inhibitors. These antibiotics block the enzyme that breaks down simvastatin, causing dangerous buildup in your blood. Even a short 5-7 day course can trigger rhabdomyolysis. If you need an antibiotic, ask for azithromycin instead-it doesn’t interact with simvastatin.
Is simvastatin 80 mg still prescribed?
It’s rarely prescribed for new patients. Since the FDA’s 2011 warning, new prescriptions for the 80 mg dose have dropped by 82%. It’s now only considered for a tiny number of patients who’ve failed all other statins and are under strict monitoring. Most doctors won’t even start you on it.
Can I drink grapefruit juice if I take simvastatin 20 mg?
No. Even at 20 mg, grapefruit juice can increase simvastatin levels by up to 260%. There’s no safe threshold. The risk of muscle damage is real at any dose. If you love citrus, switch to orange or tangerine juice-they don’t block CYP3A4.
What are the early signs of muscle damage from simvastatin?
Unexplained muscle pain, tenderness, or weakness-especially in your thighs, shoulders, or lower back. Dark, tea-colored urine is a red flag. Fatigue and fever can also occur. If you notice any of these, stop simvastatin and call your doctor immediately. Don’t wait. Rhabdomyolysis can escalate fast.
Should I get genetic testing before taking simvastatin?
If you’re considering high-dose simvastatin (40 mg or more), yes. The SLCO1B1 gene variant increases your risk of muscle damage by up to 4.5 times. Testing costs under $100 and can be done with a simple blood or saliva sample. Many insurance plans cover it if your doctor requests it. It’s one of the few genetic tests that directly changes treatment decisions.
What if I’m on simvastatin and need to start a new medication?
Always tell your doctor and pharmacist you’re on simvastatin. Ask: "Will this interact with simvastatin?" If they’re unsure, ask for a drug interaction check. If the new drug is a strong CYP3A4 inhibitor, your simvastatin dose must drop to 10 mg or less-or you need to switch to a different statin entirely. Never guess.

