Therapeutic Equivalence: What It Means and Why It Matters for Generic Drugs
When you pick up a prescription and see a different name on the bottle, you might wonder: therapeutic equivalence, the official standard that says a generic drug works the same as its brand-name version in the body. Also known as pharmaceutical equivalence, it’s the reason your pharmacist can swap a $200 pill for a $5 one without your doctor needing to rewrite the script. This isn’t marketing fluff—it’s science. The FDA requires generics to deliver the same amount of active ingredient at the same speed and intensity as the original. If they don’t, they don’t get approved.
But therapeutic equivalence doesn’t just mean the same active ingredient. It also means the same bioequivalence, how quickly and completely your body absorbs the drug into the bloodstream. A generic aspirin must release its pain-relieving compound at the same rate as the brand. Same with blood pressure pills, antibiotics, or cholesterol drugs. If absorption is off—even slightly—it can mean your treatment fails, or worse, causes side effects. That’s why the FDA tests these drugs in healthy volunteers using strict protocols. It’s not enough to look the same. They have to act the same.
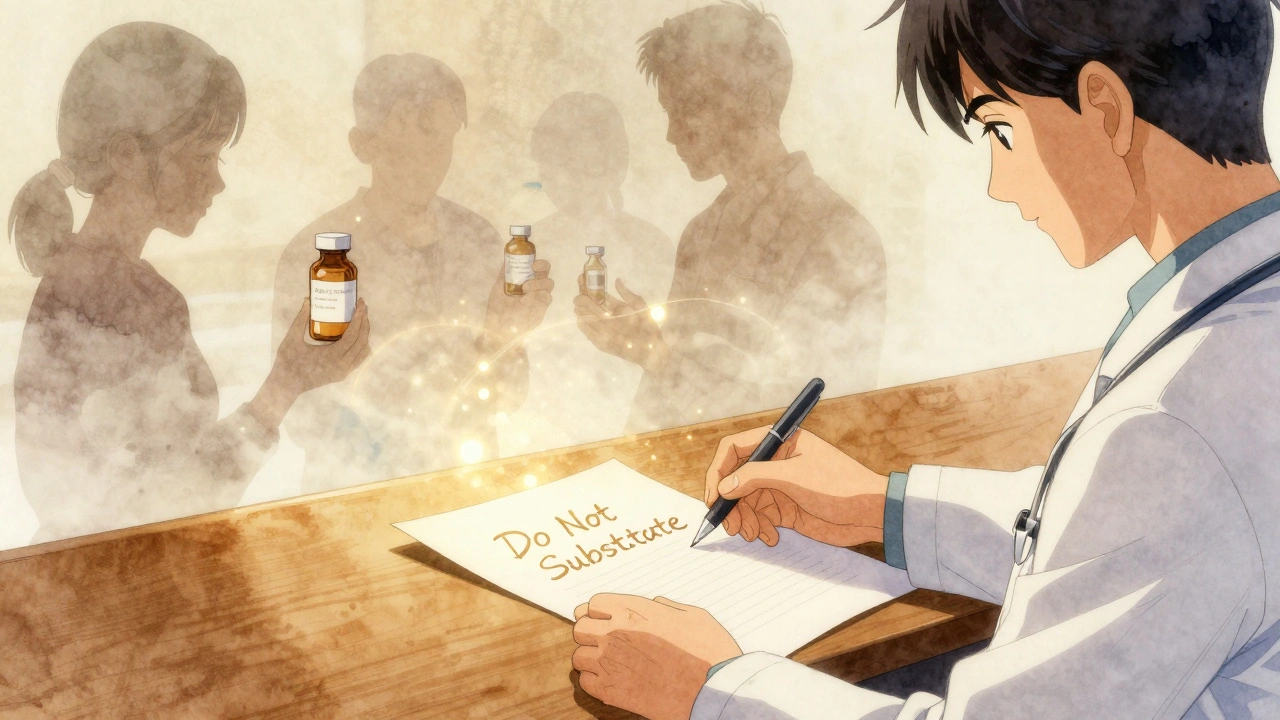
Therapeutic equivalence is what makes drug substitution possible. When your insurance pushes for generics, it’s because they’ve been rated as therapeutically equivalent in the FDA’s Orange Book. But not all generics are created equal. Some drugs, like warfarin or lithium, have narrow therapeutic windows—tiny changes in blood levels can cause big problems. That’s why doctors sometimes stick with brand names for these. Meanwhile, for most other meds, switching to a generic saves patients and the system billions every year without lowering quality.
What you’ll find in this collection are real-world stories and data-driven guides about how therapeutic equivalence plays out on the ground. From Australia’s PBS system forcing generic use to U.S. price spikes that break the system, you’ll see how policy, manufacturing, and patient outcomes connect. You’ll learn why some people get different side effects on generics, how drug absorption issues can make even an equivalent pill fail, and why certain antibiotics or thyroid meds need extra scrutiny. These aren’t theoretical debates. They’re daily decisions that affect your health, your wallet, and your trust in medicine.