When your child’s asthma inhaler suddenly looks different-maybe it’s a new color, a different shape, or the name on the label changed-you might not think much of it. But if you’re unaware, this could be a generic medication switch-a change your insurer made to save money, not your doctor. For kids, especially those on long-term medications for asthma, epilepsy, or heart conditions, these switches aren’t just paperwork. They can affect how well the medicine works, how your child feels, and even whether they end up in the hospital.
Why Generic Switches Happen-And Why Kids Are at Risk
Generic drugs are cheaper versions of brand-name medicines. They have the same active ingredient, so in theory, they should work the same. In adults, that’s often true. But children aren’t small adults. Their bodies process drugs differently. Their livers and kidneys are still developing. Their stomachs absorb things at different rates. And their weight changes constantly, making dosing more delicate. Since the 2010s, insurance companies have been pushing generic switches more aggressively to cut costs. A 2022 report from the Generic Pharmaceutical Association found that 90% of all prescriptions filled in the U.S. are generics. That’s great for the system-but for kids with chronic conditions like asthma (affecting 6.2 million children in the U.S.), it’s a different story. When insurers switch formularies, they often don’t consider whether the child can physically use the new version. A pill that’s easy for a teen to swallow might be impossible for a 2-year-old. An inhaler that works for an adult might need a spacer and mask for a toddler-and if the new generic doesn’t come with the same device, the child gets less medicine.When ‘Same Active Ingredient’ Isn’t Enough
The FDA says generics must be 80% to 125% as effective as the brand name in the bloodstream. That’s called bioequivalence. Sounds precise, right? But for drugs with a narrow therapeutic index-like phenytoin for seizures, tacrolimus after a transplant, or warfarin for blood clots-that range is dangerous. A 15% drop in blood levels might mean the drug stops working. A 15% rise might cause toxicity. A 2015 study in Pediatric Transplantation followed children who switched from brand-name Prograf to generic tacrolimus after heart transplants. On average, their blood levels dropped by 14%. Some kids had rejection episodes. Others needed emergency dose adjustments. The active ingredient was the same. But the inactive ingredients-fillers, coatings, dyes-changed. Those can affect how the drug dissolves in a child’s stomach, especially if they’re under 3 years old. Even common drugs like omeprazole (for reflux) behave differently in babies. In adults, it’s broken down mostly by one liver enzyme. In infants under 3 months, that enzyme barely works. So a generic omeprazole suspension that’s fine for a 10-year-old might not work at all in a 4-month-old. The FDA itself has pointed out that pediatric bioequivalence standards don’t exist-and they should.Small Changes, Big Consequences
It’s not just about how the drug works inside the body. It’s about how it’s taken. A 2020 study from PolicyLab at Children’s Hospital of Philadelphia found that after a generic switch, caregiver confusion led to a 15-20% drop in medication adherence. Why? The pill changed color. The inhaler didn’t come with the same spacer. The liquid tasted different. Parents thought it was a mistake. They stopped giving it. Or they gave too much because they weren’t sure. For asthma, this is especially risky. If a child’s inhaler technique drops by 50-80% because the new device is harder to use, their lung function declines. They get more coughing fits. More ER visits. More missed school days. And it’s not just asthma. The FDA lists antiseizure drugs, psychiatric meds, heart medications, and cancer drugs as high-risk areas for pediatric switching. One wrong switch can undo months of progress.
State Rules Vary Wildly-And Most Don’t Protect Kids
In 19 states, pharmacists are required to swap a brand-name drug for a generic without telling the parent. In 7 states and Washington, D.C., they must get consent. In 31 states, they just have to notify you-sometimes on the receipt, sometimes in a letter that gets lost in the mail. A 2009 study showed that when states required consent, generic substitution rates dropped by 25%. That’s not because people didn’t want to save money. It’s because families were given a chance to ask questions. To talk to the doctor. To check if the switch was safe. California passed a law in 2022 requiring Medicaid plans serving children to have a pediatric review committee before changing formularies. That’s rare. Most states still treat children’s medications like adult ones. And pharmacists? A 2018 survey found only 37% routinely discussed switching risks with parents of kids on chronic meds. That’s not negligence-it’s a system failure.What Parents Can Do Right Now
You don’t have to wait for policy changes. Here’s what you can do:- Ask before the switch: If your child’s medication changes, ask: “Is this a generic? Has it been tested in kids this age?”
- Check the device: If it’s an inhaler, nebulizer, or injector, make sure the new version works the same way. Ask the pharmacist to demonstrate.
- Monitor closely: Watch for changes in behavior, sleep, appetite, or symptoms. Keep a simple log: “Day 1: took med, no vomiting. Day 3: more coughing than usual.”
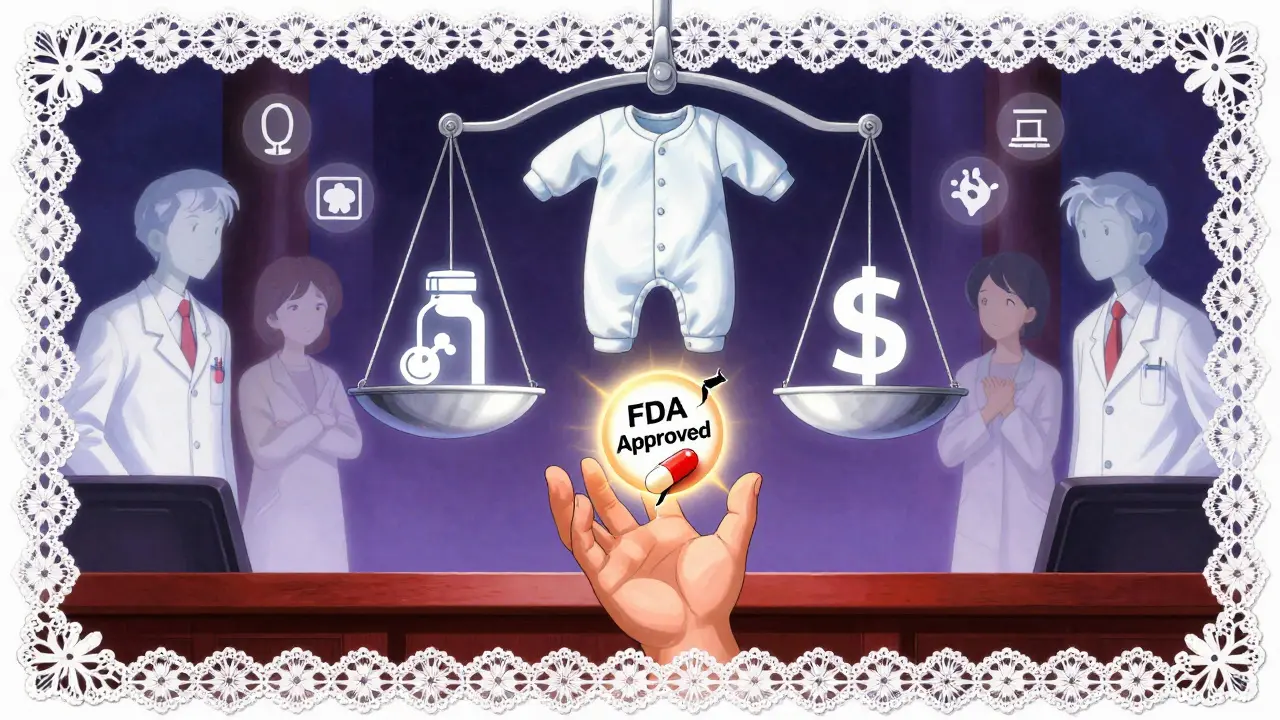
- Don’t assume it’s safe: Just because it’s FDA-approved doesn’t mean it’s safe for your child’s age. Ask for the study data. If the pharmacist says “it’s the same,” ask: “What studies prove it works in a 2-year-old?”
- Know your rights: In your state, can you refuse a switch? Call your state pharmacy board or ask your pediatrician. You have the right to ask for the original brand if it’s medically necessary.
What’s Changing-and What’s Still Missing
There’s growing pressure to fix this. The FDA launched its Pediatric Formulation Initiative in 2022 to push for better child-friendly versions of drugs. The 2023 PREEMIE Reauthorization Act included funding for pediatric drug development. The American Academy of Pediatrics is finalizing new guidelines on generic prescribing expected in late 2024. But here’s the hard truth: between 2010 and 2020, only 12% of generic approvals included any pediatric bioequivalence data. Most were approved based on adult studies. That’s not science-it’s convenience. And insurance companies? They keep switching. A 2021 UnitedHealthcare formulary change forced 23% of children with chronic conditions to switch maintenance meds. Then, when the cheaper deal expired, they switched again. That’s not care. That’s a revolving door.When to Push Back
If your child has been stable on a brand-name drug for months or years, and the pharmacy switches them without warning, speak up. Tell your pediatrician. Ask for a letter of medical necessity. Call your insurer. Keep records. If your child’s symptoms worsen after a switch, document it. Hospitalization rates for kids on switched meds are 18% higher, according to a 2023 meta-analysis in Pediatrics. That’s not a coincidence. You know your child best. If something feels off after a medication change, it probably is. Don’t let cost-saving measures override your child’s health. Ask questions. Demand answers. And if the system fails them, be their advocate.Are generic medications safe for children?
For many children, yes-especially for common conditions like ear infections or mild allergies. But for drugs with narrow therapeutic windows-like seizure meds, transplant drugs, or heart medications-switching to generics without pediatric-specific data can be risky. The active ingredient is the same, but how the body absorbs and processes it can differ in kids, especially infants and toddlers.
Can a generic drug cause different side effects in kids?
Yes. While the active ingredient is identical, the inactive ingredients-like dyes, preservatives, or flavorings-can vary between brands and generics. These can cause allergic reactions or upset stomachs in sensitive children. A child who tolerated the brand-name version might react to the generic’s new coating or sweetener.
Why do insurance companies switch my child’s medication?
Insurance companies switch medications to lower costs. Generics are cheaper, and insurers often negotiate better prices with manufacturers. Sometimes, they’ll switch back and forth as deals expire. This is called non-medical formulary switching. It’s not based on your child’s health-it’s based on what’s cheapest at the time.
What should I do if my child’s medication changes without warning?
Stop giving the new medication and call your pediatrician immediately. Check the pill or liquid for differences in color, shape, taste, or packaging. Ask your pharmacist if it’s a generic and whether it’s been tested for use in children your child’s age. Document any changes in behavior or symptoms. You have the right to request the original medication if it’s medically necessary.
Can I refuse a generic switch for my child?
Yes. In some states, pharmacists must get your consent before switching. Even in states where they don’t, you can ask your doctor to write “Dispense as Written” or “Do Not Substitute” on the prescription. You can also request a letter of medical necessity from your pediatrician to appeal to your insurance company.
Next Steps for Families
If your child takes a daily medication for a chronic condition, here’s what to do now:- Make a list of all their medications, including dosages and forms (pill, liquid, inhaler).
- Check each one: Is it generic or brand? When was the last switch?
- Call your pharmacy and ask: “Has this medication changed recently? Is this the same formulation my child has been using?”
- Ask your pediatrician: “Are there any risks with switching this drug for a generic in my child’s age group?”
- Keep a symptom journal for the next 2 weeks after any change. Note sleep, appetite, energy, and symptoms.

