Generic Substitution: What It Is, Why It Matters, and What You Need to Know
When your doctor writes a prescription, you might get a generic substitution, the practice of swapping a brand-name drug for its chemically identical, lower-cost version. Also known as generic drug switching, it’s one of the most common ways to cut prescription costs without sacrificing results. This isn’t just a trick to save money—it’s a standard part of modern healthcare. The FDA requires generic drugs to work the same way, in the same amount, and with the same safety profile as the brand-name version. So if your pill looks different but has the same active ingredient, it’s not a downgrade. It’s a smart choice.
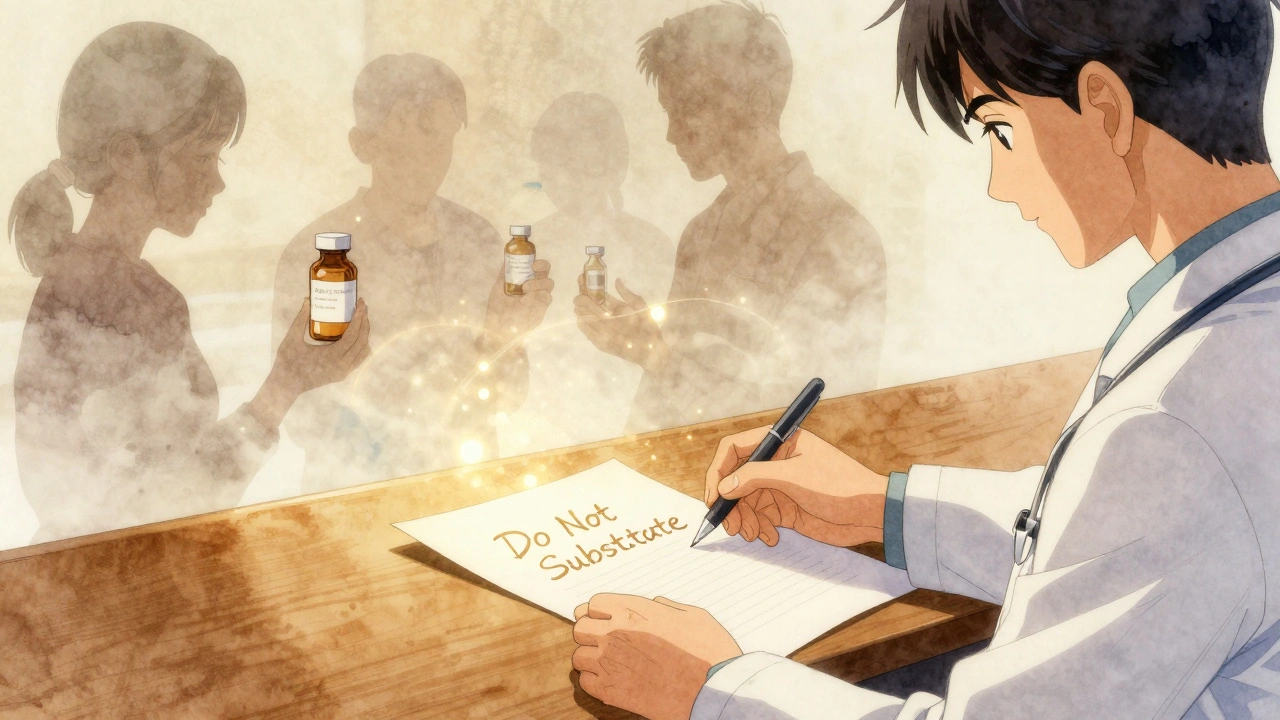
But generic drugs, medications that contain the same active ingredients as brand-name drugs but are sold under their chemical name. Also known as generic medications, they are often 80% cheaper don’t always behave the same in every body. Why? Because fillers, coatings, and how the drug is absorbed can vary slightly. For most people, that doesn’t matter. But if you’re on warfarin, thyroid meds, or epilepsy drugs, even small changes can cause problems. That’s why some doctors still write "do not substitute" on prescriptions. It’s not about distrust—it’s about control. And when you’re managing something like drug pricing, how much you pay for medications based on government rules, insurance, and market competition. Also known as pharmaceutical costs, it’s a major factor in whether people take their meds, every penny counts.
Generic substitution isn’t just about cost. It’s about access. In the U.S., generic substitution keeps millions of people on their prescriptions. Without it, many would skip doses or stop altogether because they can’t afford the brand. Medicare and Medicaid rely on it to stretch their budgets. And when new safety data comes out—like changes in how certain generics are made or new reports of side effects—it can shift guidelines overnight. That’s why you’ll see posts here about REMS programs, absorption issues, and why some generic pills work better than others. You’ll also find real comparisons: hydrochlorothiazide vs. alternatives, ezetimibe vs. statins, ampicillin vs. amoxicillin. These aren’t random. They’re all tied to the same question: When does switching drugs make sense, and when does it risk your health?
Some people worry that generics are "inferior." They’re not. But they’re not always identical in how they behave in your body. That’s why understanding medication safety, the practices and warnings that prevent harm from drugs, including interactions, dosing errors, and side effects. Also known as drug safety, it’s the foundation of every prescription decision matters. You need to know when to trust the switch—and when to ask your pharmacist or doctor to hold the line. The posts below cover exactly that: real cases, real risks, and real advice from people who’ve been there. Whether you’re switching blood pressure meds, dealing with a new thyroid diagnosis, or just trying to save on your monthly script, you’ll find the straight talk you need here.